Part 2A ~ word count 2,300
Easy-to-copy-&-share link –> http://tinyurl.com/
Is ‘elective Cesarean’ policy an effective strategy for preventing pelvic floor problems in childbearing women based on valid scientific evidence?
~ “A Scar is Born Every 39 Seconds” ~
The headline in a 1998 advertisement for a skin product
to rub on C-section incisions to diminish scarring
Ob.Gyn.News April 15, 1998
This statistic — a ‘scar’ is born 39 seconds — referred to the number of Cesareans performed in 1995, when the Cesarean rate was a mere 20%. Imagine what the rate of Cesarean ‘scars per second’ rate in 2019, with a 32.8 % rate or 1.3 times higher?
-
The inability of Cesarean surgery to prevent pelvic floor problems in childbearing women is well-documented
When what you see is not what you get!
There are many published studies that refute the notion that Cesarean surgery effectively reduces or eliminates what used to be called “females troubles” — pelvic floor problems that include incontinence, uterine prolapse, and related issues.
However, nothing I could say about the false strategy of using ‘elective’ Cesareans to prevent ‘female troubles’ could possibly be more informative or authoritative than the following two excerpts.
Documentation ~ Published studies and professional warnings to obstetricians by obstetricians
The first is from “Elective C-section Revisited” by Sacramento obstetrician Dr. Elaine Waetjen (Ob.Gyn.News; August 1, 2002, Vol 36, No 15):
The prophylactic use of elective cesarean section to prevent pelvic organ prolapse and urinary incontinence is gaining increased attention.
Dr. Benson Harer, Jr, past president of the American College of Obstetricians and Gynecologists, stated publicly last year that women should have the right to choose a cesarean delivery.
“….why shouldn’t we offer prophylactic C-section to prevent this problem later in life?”
The answer is that the evidence does not support this approach. Preventive strategies should cause no more harm than the disease or problem that they are trying to prevent. Ideally, they should:
-
- incorporate some kind of screening to identify people at risk
- they should be cost effective
- based on very good evidence of benefit
Elective C-section to preserve pelvic floor function fails on all these measures.
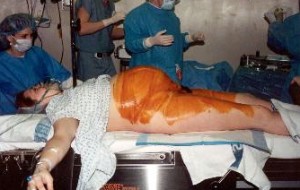
“Cesarean surgery causes more maternal morbidity and mortality than vaginal birth. In the short term, C-Section doubles or triples the risk of maternal death, triples the risk for infection, hemorrhage, and hysterectomy, increase the risk of potentially-fatal blood clots 2 to 5 times and causes surgical injury {to the baby} in about 1% of operations.
In the long term, cesarean section increases the mother’s risk of a placenta previa, accreta or percreta, uterine rupture, surgical injury, spontaneous abortions, and ectopic pregnancies while decreasing fecundity {i.e. infertility}.
Babies delivered by cesarean have a higher risk of lung disorders and operative lacerations.” Cesarean babies also have triple the rate of asthma as adults. (*Cesarean Birth Associated with Adult Asthma — ObGynNews, 6/15/01, Vol 36, N0. 12)
…would have to do 23 C-sections to prevent one such surgery {for organ prolapse or incontinence} later in life.
So instead of offering elective cesarean in an attempt to prevent future prolapse or incontinence, we should be examining what we can do in our management of vaginal deliveries to protect pelvic floor function”.
The second excerpt is from Elective Cesarean Section:An Acceptable Alternative to Vaginal Delivery? by Dr. Peter Bernstein, MD, MPH; Associate Professor of Clinical Obstetrics & Gynecology & Women’s Health, Dept of Obstetrics & Gynecology, Albert Einstein College of Medicine, New York; Medscape ~ Ob/Gyn & Women’s Health 9/16/02
“One argument often cited in favor of elective cesarean delivery is the prevention of pelvic floor damage, which can occur with vaginal delivery. Stress urinary incontinence, pelvic organ prolapse, and anal incontinence have been associated with vaginal delivery.
But these adverse side effects may be more of the result of how current obstetrics manages the second stage of labor.
-
- Use of episiotomy and forceps has been demonstrated to be associated with anal incontinence in numerous studies.
Perhaps also vaginal delivery in the dorsal lithotomy position with encouragement from birth attendants to shorten the second stage with the Valsalva maneuver [prolonged breath-holding], as is commonly practiced in developed countries, contributes significantly to the problem.
Nonetheless, the prevention of pelvic floor injury by routine elective cesarean delivery is not an appropriate solution. Rather, more research into the management of the second stage of labor is clearly necessary. Moreover, cesarean delivery does not guarantee protection against pelvic floor dysfunction, given the reports of similar rates of urinary incontinence in nulliparous woman as in parous women [2]
A potentially more persuasive argument in favor of elective cesarean delivery is based on the potential for fetal risks before and during vaginal delivery, including intrapartum death, intrapartum acquired hypoxic-ischemic encephalopathy, and stillbirth at term before the onset of labor.
What is not clear, however, is how many cesareans would have to be performed to avert these disastrous events and what the cost would be in terms of maternal morbidity and mortality in order to prevent a single untoward fetal outcome.
To suggest that performing an elective cesarean delivery in a low-risk patient will avert intrapartum fetal injury is very misleading. These outcomes are rate, even in higher-risk women.
Indeed, they are so rare in women without any identifiable risk factors that an absurd number of cesarean deliveries would need to be performed to avert even one of these poor outcomes. Thus, resorting to cesarean delivery would not be an appropriate standard procedure.
Although cesarean delivery has clearly become safer over the past 50 years with advances in antibiotics, anesthesia, and thromboprophylaxis, it is still not without risks. Woman undergoing cesarean delivery have greater blood loss and risk of damage to internal organs. The mortality risk of undergoing an elective cesarean delivery with no emergency present has recently been reported almost 3 times the risk of vaginal delivery. [3]
In addition, risks to the fetus associated with a cesarean delivery range from lacerations [a cut in the baby’s face or head when the surgeon makes the incision into the uterus] to respiratory distress syndrome and transient tachypnea of the newborn. Although these are typically manageable, their cost will be multiplied many times over if more elective cesareans are performed.
One of the most significant risks of cesarean delivery is the need for a subsequent cesarean delivery. … A repeat cesarean delivery carries significantly more risk in terms of placenta previa, placenta accreta, uterine rupture, injury to internal organs during surgery excessive blood loss, need for hysterectomy and maternal death.
These risks rise with each subsequent repeat cesarean delivery. Risk of [placenta] accreta and previa increases with each subsequent cesarean delivery, increasing to 60% in women with 4 or more cesarean deliveries. [4] In addition, the incidence of emergency peripartum hysterectomy for abnormal placentation seems to be rising as a result of the increased rates of cesarean delivery.
A move toward routine elective cesarean delivery may also have significant costs in terms of lost opportunities for bonding between mother and newborn. A woman who has had a cesarean may be less able to care for her child and may have a more difficult time breastfeeding
….. Although this impact may be small for the individual patient, again, its costs multiplied over a large population may be great, based on the accumulating evidence for the benefits of successful long-term breastfeeding.
Arguments made by proponents of elective cesarean that it should only be provided to women who intend to have only 1 or 2 children fall flat, given that the rates of unintended pregnancy in the US approach 50%. And what of the woman who changes her mind 10 years later and chooses to have another child after having had 2 prior cesareans?
There may be no legal liability to the physician who performed the patient’s first cesarean section when the patient winds up with a hysterectomy or worse, but that does not clear that physician of responsibility for performing a surgical procedure of unclear benefit upon a patient’s request.
Some argue that, from an ethical point of view, allowing a patient to choose to deliver by cesarean is not substantially different from allowing her to choose to undergo cosmetic surgery.
But cesarean is very different. The benefits of elective cesarean relative to vaginal delivery are not established and the risks are substantial, especially given the potential for future repeat cesareans.
That women are seeking elective cesarean deliveries is probably more significant in that it indicates the failure of modern medicine and society at large, in the sense that women may fear the experience of labor and birth attendants may fear the legal risks of allowing appropriate women to have a trial of labor.
Modern management of labor should be reassessed to address the concerns raised by proponents of elective cesarean delivery. If elective cesarean becomes an acceptable alternative, we may never be able to undo the practice.
Excerpts from “Elective Cesarean Section: An Acceptable Alternative to Vaginal Delivery?” by a clinical professor of obstetrics and gynecology, Dr. Peter Bernstein, MD, MPH; 9/16/02
Failed Medical Experiment:
How the policy of using C-EFM as the obstetrical Standard for all childbearing women is related to our sky-rocketing C-section rate and its many complications
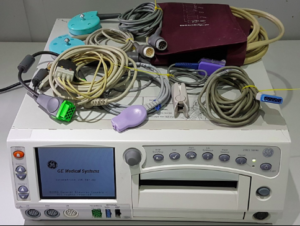
The current EFM technology was invented in 1969, but not widely adopted until the mid-1970s. In 1970, the C-section rate was 3%-5%. By the 1980s, it had sky-rocketed to 25% and now is 33%
And yet, the consensus the professional studies and journal articles, starting in 1975, is simple and straightforward: The policy by the American obstetrical profession of continuously monitoring all laboring women and performing emergency cesareans based on “non-reassuring” EFM tracing is a failed medical experiment.
This undeclared medical experiment was based on a hypothesis that continuous electronic monitor of all labor patients would virtually eliminate cerebral palsy and perinatal morbidity and mortality, thus reducing the financial burdens on families and the taxpaying public by virtually eliminating the incredibly expensive care required for children with CP and permanent neurological damage.
As quoted in the previous post, an article written by an obstetrician for other obstetricians and published in 2011 (The Female Patient “Electronic Fetal Monitoring Update”:
“Despite the widespread use of EFM, there has been no decrease in cerebral palsy.
… a meta-analysis of randomized control trials has shown that EFM has no effect in perinatal mortality or pediatric neurologic morbidity.2
However, EFM is associated with an increase in the rate of operative vaginal and cesarean deliveries.1”
These have always been extremely worthy goals, and I personally hope we can figure out how to achieve them, the sooner the better. But when it comes to c-EFM, the scientific literature does not provide the “proof of theory” so desired by hospital chains and the obstetrical profession because universal use of c-EFM does not achieve its own goals when applied to the 70-85% of healthy childbearing women with normal pregnancies.
Instead of helping healthy childbearing parents and society, its routine use results in expensive iatrogenic complications that primarily affect the childbearing woman, in particular, an increased rate of morbidity and mortality that is extraordinarily expensive for society and painful if not tragic for families.
All this is a direct result of the higher Cesarean section rate and its propensity for spawning complications during the surgery itself, immediately post-op and/or serious delayed and downstream problems for both mothers and babies.
The ethical high road: Admit and correct mistakes
The history of western medicine includes dozens of policies and highly regarded medical treatments that were ultimately proven to be ineffective, harmful or both. For the most part, these researchers and developers were highly ethical people motivated by a genuine desire to advance medical science, reduce suffering, and prevent untimely deaths.
It’s normal for inventors of a new or improved medical treatment or medical device to be excited about them and more focused on their potential benefits than possible risks and negative side-effects. Nonetheless, its a fact of life that many of these new policies or protocols, new drugs or medical devices turn out to be ineffective or harmful.
When that happens, developers and manufacturers of these new medical treatments have to acknowledge the harm and stop promoting their product or process in its current form.
An example of admitting and correcting a mistake is the story of a new therapy introduced in 1947 for premature babies. This treatment consisted of piping high concentrations of oxygen into the baby’s incubators over long periods of time. By 1952 — just 5 years later — over 7,000 premature babies had been blinded as a result of this new oxygen therapy. What seemed like a really good idea actually caused irreversible damage to the eyes of these babies that resulted in permanent blindness. [1]
This new iatrogenic condition was originally called retrolental fibroplasia but is now referred to as “retinopathy of prematurity” (ROP). A close friend of our family was one on those premies. His parents were assured that their baby was getting the most up-to-date treatment and they had nothing to worry about but the high levels of oxygen left him totally blind. A more well-known victim of RLF is the famous musician, Stevie Wonder.
One study reported that in developed countries, the oxygen toxicity accounted for 10% of the case of childhood blindness.
But the medical profession realized what was happening and corrected the problem. As a result, high concentrations of oxygen are no longer the “standard of care” for all premature babies.
But so far the American obstetrical profession has steadfastly refused to admit that their policy identifying c-EFM as the universal standard wrong: c-EFM for healthy low-risk mothers is ineffective, introduces unproductive expense, and results in a statistically-significant increases the C-section rate and exposes these new mothers to the serious risks of Cesarean surgery and all its delayed and downstream complications.
Continue: ~ 2B ~ Part 2B~More on Cesareans and simple explanation of how Auscultation works ~ 2B
References for retrolental fibroplasia
1. The Permanente Journal