The Brave New World of Evidence-based Maternity Care for 21st Century ~ Chapter 2
Chapter 2
The Church of Obstetrical Medicine:
Obstetrical nursing during the “dark ages of the deep south”
~ My professional background, personal story and preamble to evidence based practice
faith gibson, LM (2005)
 As a nurse and a midwife over the course of four decades, I learned the ropes of obstetrical nursing and normal maternity care in a racially segregated Florida of the early 1960s.
As a nurse and a midwife over the course of four decades, I learned the ropes of obstetrical nursing and normal maternity care in a racially segregated Florida of the early 1960s.
I got to closely observe and directly participate in two entirely different systems, side by side in the same hospital, at the same time, same staff, same type of patients, totally different management, dramatically different outcomes. It was a profound, one-of-a-kind education in sociology of racial prejudice as well as the prejudice of the medical profession against physiologic childbirth practice.
In addition to technical skills associated with labor and delivery room nursing, and I also learned, a one-of-a-kind natural study contrasting these two styles.
I was an incredibly young (right out of high school) and naive student nurse in 1962 from a family that did not acknowledge human biology, whether this related to the biological functions of sexuality or childbearing.
I hadn’t figured out exactly where (i.e. which orifice) the baby came out when I was exposed to circumstances and situations as a student nurse that were life-changing that ran the gambit from the ridiculous to the sublime. One of the best and most useful aspects of my training were the stories and wisdom imparted to our first year class by the director of our nursing program, Etta McLaughlin.
She had trained as an nurse in NYC at Mt Sinai Hospital in the 1930s and from our perspective, “had seen it all”. In the post-antibiotic world of the 1960s Miss Etta could relate stories of what it was like to attempt to treat diseases such as pneumonia, post-operative infections, TB and syphilis in a pre-antibiotic era. We students quickly developed an abiding loyalty to the “miracles” of modern medicine”, impressed by her stories of what it was like to stand by and watch people die because there was no effective treatment for common but nonetheless potentially-fatal infections.
Professionally speaking, Miss Etta was “old school” to the core. She wore her starched and spotless nurse’s uniform and organdy nurse’s cap with such dignity that she was a larger-than-life inspiration to us all. We hung on her every word and wanted to emulate her style. To me, nursing was a form of religious vocation – a “calling” to a noble pursuit with high ideals.
I wanted to go to Africa and be a nursing nun just like Audrey Hepburn in the “The Nun’s Story” and save mothers and babies from the horror of their primitive circumstances, such as being denied the hospital-based care of physicians and instead forced to give birth in a dirt-floor hut with a granny midwife who didn’t even know to wash her hands or sterilize the birth instruments.
But what impressed me the very most were two things Miss Etta said during the early weeks of our training program.
The first was a definition of what it meant to be a healthcare “professional”, which was that as a doctor or nurse, we would be expected to put the well being our patients above our own. That included our own physically safety, as nurses and doctors are required to care for those with untreatable contagious disease, acting out alcoholics and violent psychiatric patients.
But it also meant putting the welfare of our patient ahead of our own concern for personal convenience, economic advantage or professional career development. TO be ‘professional’ meant to do the right thing even when it was inconvenient, hard, dangerous and/or not ‘profitable’. It meant doing the ‘right’ thing simply because it was the right thing to do – a behavior that was true to our word and that honored the ‘honorable’ humanitarian profession of medicine.
One of the examples Miss Etta gave was a patient that had a cold virus insisting that his doctor prescribed antibiotics, even though the doctor was well aware that antibiotics are both ineffective and counter-productive against viruses.
By this definition of “professional” duty, his doctor would be obligated to decline the request for antibiotics, even if the patient got mad and stormed off to get his antibiotics from a different doctor. This “professional conduct” extended to nurses and their obligation to protect the patients from all manner of dangers – including contagion, infectious material, wrong drugs and a duty to advocate for the patient’s safety even when that meant going against the “powers that be” – head nurses, hospital administrators and the hubris of certain surgeon types, famous for their arrogance.
A Pearl of Great Price
Miss Etta’s second important lesson was related to us in the form of a little story about an elderly peasant woman who was a fish vendor in a 3rd world village.
On every market day, the peasant woman sat at a small table with a big bucket at her side, filled to the brim with a shiny and undulating mass of very lively eels. In preparation for their sale, she reached down and randomly grabbed a writhing eel and then used two large straight pins to tack down each end of the eel to her cutting board. Next she deftly used her knife to slit its body from end to end and removed the meat.
Everyone in the village was used to seeing this and didn’t think much about it. Then a stranger came by one day and after watching her for a few minutes, asked if it wouldn’t be more humane to kill the eels first, or at the very least knock them unconscious before slitting them open.
She replied “Why I’ve been doing this for 20 years, they ought to be used to it by now”.
Of course the moral of the story is that healthcare professions do fear-provoking and painful things to patients everyday. However familiar these routines may be to the doctor or nurse, they are still anxiety provoking and painful to the patient. It was a story that has had a profound and continuing effect on my practice as a nurse in the maternity wards and the emergency rooms and later on as a mother and now as a community midwife.
Shocking realities as a student nurse
Insightful as these charming stories were, an awful lot of my nurses’ training was shockingly awful experience for an 18 or 19 yr old with so little life experience.
I remember trying to provide nursing care to a 45 year old woman dying of cancer, who had a colostomy and a stem-to-stern abdominal incision that had eviscerated (broken open). It was my job to poke sterile gauze into this messy, foul-smelling wound that would never heal, while her colostomy kept running like a river, defying my best efforts to keep anything sterile. Sadness sweeps over me again just recalling this heartbreaking incident.
I want to cry for both of us – this nameless, helpless, hopeless woman who laying dying all alone in a charity ward with me, the inexperienced and overwhelmed 18 yr old student nurse, her only help in times of such grave trouble. On her behalf, I have never quite forgiven God.
Clinical training at the Sunland Training Center, Orlando
Another major trauma of my training was the several weeks in pediatrics that I spent at a huge hospital for profoundly disabled children. An old TB sanatorium with enormous open wards and floor to ceiling windows, known as the Sunland Training Center (outside of Orlando, Florida), had been converted into a hospital that provide custodial care for the youngest, sickest children with most profoundly broken minds and bodies.
This building housed over a 1000 of these special “kids”, ages newborn and up. Most were diapered babies and incontinent children under the age of 12, so developmentally disabled that they were either tube fed or had a tasteless, unappetizing blender food (actually a brown-gray gruel) spooned into them three times a day by over-worked and under paid nurses aids. The majority of these children spent 24 hours a day confined to metal cribs with tall bars, lined up in neat rows of 30 on each side, 60 to a unit, two units to each floor, an overwhelming 6 floors in all.
Each day we lined their cribs up like a long wagon train snaking around the room in preparation for communal bathing. Nurses working in teams of two stripped them naked and washed them on a porcelain slab in the center of the room with a hose in a manner more reminiscent of dog grooming. Other nurses changed the bed linens and then dried, diapered and dressed each freshly cleaned infant or child and plopped him or her back in their cleaned crib.
Some of the kids had awful, disfiguring physical anomalies, others were physically perfect but had a mental age and development of a newborn – innocent beauty that housed a vacant stare. Some were functionally impaired with heart defects, blindness, were deaf (or all three).
I particularly remember a beautiful, dark-haired 12 yr old girl with smooth alabaster skin that I call “Pumpkin”. She had the mental age and ability of a 7-month fetus, but a body that was turning her into a young woman with budding breasts, a permanently “Sleeping Beauty” for whom the kiss of a lover will never awaken. I felt so sorry for her mother, to see her daughter growing more lovely each day while trapped forever in the suspended animation of life-long neurological damage.
I was simultaneously horrified and fascinated this. I burned with a desperate need to understand how this could have happened – Was Mother Nature a really just a b-i-t-c-h? was it bad genes, bad nutrition, bad luck, lack of access to medical care?
I had to know more, so I read the chart of each and every child on our floor – more than 60 — and discovered three major categories that explained the majority of cases. The most frequent causes were apparent at or soon after birth — congenital anomalies (such as spina bifida, hydrocephalus).
Second was maternal infections during the early weeks of pregnancy (rubella or German measles, which causes the above mentioned trilogy of heart defect, blindness and deafness).
And third were birth injuries – damage caused by or occurring during the intrapartum period (labor and birth).
A fourth category, which only accounted for a tiny fraction of these children, had suffered infections (such as meningitis) or been hurt in a bad fall or car accident.
As a student nurse who aspired to future motherhood, I was particularly interested in the category of “birth injuries”. I hoped to learn something that would be “protective” for me and my future family. In my nurses’ training I had not yet rotated thru obstetrics and continued to be intensely curious about childbirth. About half of the patients on our floor, or 30 out of 60 kids, had charts with a diagnosis of “birth injury”. They described such things as premature birth, very low birth weight, precipitous or purposefully obstructed delivery —“mother says nurse held the baby back until doctor arrived”, long labor — difficult forceps delivery, uterine rupture subsequent to induction, or “mother given a large quantity of narcotics just prior to delivery, baby severely depressed at birth, was resuscitated, low Apgar scores, postnatal seizures”.
I recall one chart in particular that described a general anesthesia accident in which the mother stopped breathing. Both she and her baby were brain damaged by the event and now required custodial care in two different hospitals. There were two older children left with the father, who visited only occasionally.
I was surprised at how many of these so called “birth injuries” were actually preventable and represented lack of appropriate care, poor care or incompetent care. This included neglected labors (“doctor refused to come in for three days”), excessive use of drugs (“mother given 15 doses of narcotics over a two day period”) or were the result of nurses protecting themselves from the criticism of doctors (and possible lost of their jobs) by holding the mother’s legs together to keep the baby from delivering before the doctor arrived.
Nowadays we would categorize this damage as “iatrogenic” – medical or nursing care that is the direct or indirect cause of injury or death – i.e., malpractice. But suing doctors was extremely rare in the years preceding my student nurse experience and so doctors got away with a lot.
One must conclude that current, high-level threat of malpractice litigation prevents at least some of those preventable birth injuries. As for congenital anomalies and other malformations caused by maternal infection, we can prevent many of them through pre-conception immunization against rubella. Genetic testing and ultrasound imaging also picks up many of these problems prenatally.
Mercifully this distressing student rotation came to an end and I was sent back to the main teaching hospital (“Orange Memorial”, since then renamed “Orlando Regional”). While rotating through the OR, I got to see my first baby delivered – a Cesarean section of course – and was flabbergasted.
For some strange reason I was surprised that the baby came out all “finished” – a totally formed, perfectly lovely baby girl. Although it sounds absurd to say, I thought a newborn baby would begin as a little shapeless blob — some sort gelatinous gue — that would be taken to the nursery and after several days of special care, be presented to the parents as a finished product, ready to be taken home.
Finally the long awaited day came when I rotated to the obstetrical unit. This was an enormous relief to me, as the difficult and complicated care required by medical and surgical patients was both upsetting and taxing. And the heart-wrenching cases I worked with in pediatrics — 3 year olds dying of brain tumors or having been scalded by abusive parents — were more that I could bare.
These high-anxiety situations were always accompanied by the constant refrain from our nursing instructors that there were a “1000 way to kill a patient without ever even entering their room” (ordering the wrong drugs, failing to give the right drug or dose, etc). As a shy 18 yr old, giving a bed bath to adult men was highly distressing, especially the obvious question of bathing ‘certain parts’ or ‘you know, down there’.
In our student nurse world by Miss Etta explained this to us in a little homily (note to self: lookup this word). The instructions to us in regard to bathing male patients were to ‘bath down as far as possible’ without bumping into a certain appendage, wash up from the bottom as far as possible, again avoiding the aforementioned appendage and then hand the warm soapy washcloth to the patient and instruct him to bath “possible” while we demurely stepped out of the room.
However maternity patients are, thank heaven, all female, can be expected to be generally healthy and therefore not be suffering from some awful disease or likely to die. I anticipated that the work would be happy – lots of new moms and new babies, proud papas, cigars being passed around, Champagne and balloons. What was not to like!
Not only was the work pleasing, but I felt that it was also holy. It seemed that somehow the mysterious off-limits delivery rooms – actually sterile operating rooms — were the ‘holy of holies’ and the next thing to an alter upon which the central and sacred act of human reproduction — giving birth — was to occur, attended by the high priests of childbirth — obstetricians and their faithful handmaidens, labor and delivery rooms nurses. I aspired with my whole heart to become part of that sacred ritual.
Having so recently came from my rotation through the Sunland Training Center and stared every hour into the face of what happens when good obstetrical care is absent, unavailable or in any way deficient, I expected that our doctors and nurses would be ‘angels of mercy’. They would above all protect mothers and babies from all the awful birth-related damage I had seen. In my mind those problems were associated with the “bad old days”, things that happened 5 or 10 years ago (for an 18 year old, ten years is half a life-time!) when most of those children in the Sunland hospital had been born.
I assumed that obstetricians had been as horrified as I was at the tragedy of these preventable birth injuries and that all these iatrogenic causes had been identified and promptly eliminated. Surely our doctors and nurses would never give too many drugs or hold any mother’s legs together to keep her from giving before her doctor arrived or do anything else that would introduce unnecessary harm into the picture.
During the first hour of the first day of my first rotation through the labor and delivery room, at exactly 7:25 in the morning, while I was still being “oriented” to the unit, a young “unwed” mother was wheeled through those swinging double doors that grace every L&D in the western hemisphere. Sitting crookedly in the wheelchair, it was immediately apparent that she was very far advanced in labor (the pushing sounds were a real give-away!). I was so excited as the charge nurse practically threw this mother-to-be on to a gurney and together the three of us raced the stork down the hall and into one doorway of the double delivery room.
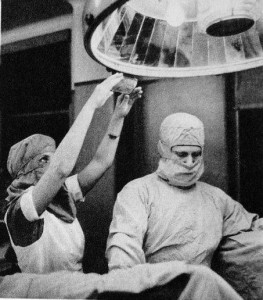
At that time our delivery rooms were typical of the era, that is similar to the operating rooms portrayed on the TV show M.A.S.H. – a single large room with two operating tables and anesthesia machines, separated by a folding screen that was placed in the middle so the patients on each table could not see one another. Doctors and nurses often slipped back and forth between two simultaneous deliveries, proving assistance wherever it was needed most.
On this particular day there was already a delivery in progress on the other side of the delivery room. As we came loudly crashing into the empty side of the double set-up, the nurse anesthetist from the delivery-in-progress came around the screen and quickly sized up the situation. She immediately reached for the anesthesia equipment, turned on the Cyclopropane anesthetic gas and came around to the head of the gurney with the black face mask in hand, ready to provide the “blessed relief” of unconsciousness.
At this point the laboring woman on the stretcher couldn’t see nurse anesthetist, who was behind her and out-of-sight. So it was a great shock to the mother when an anesthesia mask seemed to fall from the sky and be pressed firmly over her mouth and nose and cutting off her air. As could be expected, this young women – really just a girl of 16 who had probably never been a patient in a hospital ever before – began to struggle and claw at the facemask, trying to remove it, while the nurse anesthetist continued to chase her bobbing head around the top half of the stretcher. As this strange struggle was playing out, the CRNA said:
“Oh honey, you’ve got to have this, it hurts too bad not to, you couldn’t stand it”.
At this precise moment, the OB resident who had been paged “Stat to the delivery room” over the hospital loud speaker (in the days before packet pagers!) showed up on the run. Standing at the foot of the stretcher, slightly out of breath and surveying the scene, he barked, in a none-too-friendly voice, “Oh let her go, she’ll know better next time”.
On the very next push, the baby just slipped out, with no fuss or effort by this 16 year old who gave birth so easily, with no outward signs of pain or difficulty. This was followed by a crystal clear moment of what is known as ‘cognitive dissidence’ – my eyes and my ears were assailed by a competing and incongruous story. If one was true, the other had to be false.
These two seasoned birth professionals — a nurse anesthetist and OB resident — had both just equated normal childbirth to intolerable pain requiring general anesthesia and alluded to extraordinary regret by the mother-to-be for being so “foolish” as to refuse it. Yet what I had seen did not look like a train wreck – no yelling, no writhing in pain, no blood, no gaping wound, nothing but the perfect miracle of that slippery little head peeking out timidly at first, followed immediately by the baby’s whole body, feet and the umbilical cord trailing along behind. I remember the large pink pool of steamy amniotic fluid and how the cord glistened as the baby lay there on the stretcher between the mother’s legs, a perfectly formed 7 ½ pound baby girl.
It was my very first vaginal birth and I was too “green” to appreciate the significance of the umbilical cord’s quiescence, its smoothness, it’s pale, slender and oh-so-still walls. You see, in a live baby, the umbilical cord is as big around as your thumb, purple and spirals like a fat phone cord that pulses with every beat of the baby’s heart for several minutes after the birth.
On this day, the umbilical cord was not the only thing that was still and quiet. The baby did not move, did not cry, did not try to breathe, did not have a heartbeat.
Afterwards, when the shocked and grieving mother was moved out of the delivery room, on the same stretcher upon which she had given birth, I asked the wise older nurse “why?” Why would cause this perfect little baby be stillborn? She said “some babies just don’t make it, nobody knows why”. With that she turned and with quietly dignity walked off to resume her duties as a humble servant in the Church of Obstetrical Medicine.
Hospital Childbirth-Southern Style 1960s
In the 1960s, “Southern-style” childbirth in the ‘Deep South’ (Orlando, Florida) depended on your color. For white women, it was “knock’em out, drag’em out”, a combination of narcotics, general anesthesia, ‘generous’ episiotomies, ‘outlet’ forceps, manual removal of the placenta, lots and lots of stitches to close the large perineal incision and return the vagina to “virginal” status and afterwards, the routine separation of mother and baby for the first 12 to 24 hours. For black mothers it was as different as night and day.
Caucasian women were admitted to the all-white 5th floor Labor and Delivery unit known as 5 North, tucked away at the end of the hall between the nursery and the north elevator. It was an old-fashioned a five-bed labor ward with 2 delivery rooms, originally built in the late 1940 or early 1950s. The only privacy was hospital-type hanging curtains between each bed. If a Cesarean section became necessary the woman had to be moved by stretcher two floors down in the north elevator to the surgery suites.
The first stop for each new labor patient, after kissing her husband or other family members good-bye, was the “prep room”, where she was first examined by a resident and if determined to be in active labor, given the standard obstetrical prep (full pubic shave and large soapsuds enema). This medically-unnecessary ritual of hospital labor and delivery was a left over from the early part of the 20th century.
Pubic shaving started when many poor patients in charity hospitals were discovered to have pubic lice. Giving laboring women a large soapsuds enema on admission and repeating it every12 hours was done in the mistaken belief that the big killer of childbearing women — childbed fever or puerperal sepsis — was caused by “auto-contamination”.
The notion was that deadly disease germs that killed so many new mothers had originated in the woman’s own alimentary canal and contaminated the sterile operative field during the birth. Wrong. This potentially fatal streptococcal infection is an iatrogenic or nosocomial disease caused by doctors, nurses or other hospital staff or from contact with contaminated surfaces. The infection was spread to newly delivered mothers on unclean hands of physicians, hospital staff, dirty linens or unsterilized surgical instruments. The hot soapy water used for enemas was tragically misplaced — it should have been used to clean the hospital rather than irrigate and irritate the colons of labor patients.
While the newly admitted mother-to-be was being subjected to uncomfortable and distasteful prepping procedures, she might well be startled by the piercing screams of several different heavily medicated laboring women just across the hall. An anxious look would come across her face as she asked in a frightened voice “What’s wrong with them?” It was my sad duty to tell her these screaming women were “just having a baby”.
The next stop for the newly admitted labor patient was to be put to bed in a closed unit that did not permit husbands or other family members to visit, no matter how long she might be in labor. The mother-to-be was immediately given a double dose of sleeping pills and after that she was NPO – no food or water until after the birth, no matter how long that might be. Next she was injected with a huge dose of narcotics (100 mg of Demerol) mixed with a psychotropic drug (20 mgms Lorfam, Vistaril or Valium) and the amnesia and hallucinogenic drug scopolamine (1/150 grains), to be repeated every 2 to 3 hours during labor (no matter how many times), until the baby was born, even if it took a couple of days (or longer).
These women were so “knocked out” that they drooled and talked in nonsense syllables. With every uterine contractions they rose up out of the bed, made low moaning sounds or shrieked in pain and ask over and over again “what’s happening, what wrong with me?” as the amnesic drug made them forget they were in labor. We repeatedly told them they we OK, they were just in labor and it would soon be all over but they didn’t remember the explanation either.
This went on for hours on end. Under the influence of these powerful hallucinogenic drugs some women became temporarily psychotic and physically fought with the staff. They bit nurses or doctors, fell out of bed, chipped teeth or broke an arm. To prevent falls (and lawsuits) a nurse was obligated to stand or sit right by the bed, no further than an arm’s length away. If the unit was too busy to spare a nurse for one-on-one custodial care, then these women were put under four-point restraint – heavy leather wrist and ankle cuffs designed for use in psychiatric hospitals. These were clamped to both arms and legs and then buckled to the four corners of the bed, holding the mother spread eagle on her back.
The use of four-point restraints was considered fortunate by the doctors because they believed that since labor hurt more when women were on their back (this was obvious to all observers), that uterine contractions must be more effective when the mother was on her back. Doctors often ordered the nurse to keep a labor patient on her back as a strategy for accelerating labor in an era before the use of Pitocin was common.
The other ‘advantage’ of wrist restraints was that it kept these heavily medicated women from touching themselves “you know, down there”. One of the effects of the amnesic drug scopolamine was to produce the pharmaceutical equivalent of a lobotomy – that is, to liberate the mother from all her normal inhibitions.
The observed behavior of thousands of heavily medicated women in active labor by hundreds of L&D nurses is that the ‘natural’ inclination of these women was to respond to the pain of uterine contraction and especially the pressure of the baby coming down the birth canal by pressing their fingers against top half of their public region and wiggling or rubbing. Observers of this behavior often mistook or mislabeled it as masturbation.
Of course, this direct association between childbirth and ‘raw sex’ was something the staff found shocking and spoken about in disgusting tones. This personal revolution seemed to renew the efforts of many of the staff to keep such women in wrist restraints for the balance of their labor. It was seem as an all purpose solution — prevented women from falling out of bed, forced them to labor in the most non-physiological posture possible (with the exception of being held aloft by their heels!) and also made it impossible to touch their own genitals.
{Tag ~ tell story of maternal toe-spreading frequently associated with pushing, and also noting this same reflex is associated with sexual orgasm}
When the birth became imminent, the labor patient was taken to the delivery room on a stretcher and dragged or pushed by two or three nurses over to the delivery table. Still under the influence of psychotropic and hallucinogenic drugs, the mother’s arms were immediately tied down in big leather wrist restraints on each side of the delivery table. The rationale for this was both to prevent her from falling off the narrow table and also to keep her from touching her crotch or any of the sterile drapes or instruments used during the “surgical procedure” of a vaginal delivery.
Her legs were then placed in obstetrical stirrups and secured with leather straps that buckled over the thigh and calf of each leg. At this point the table was “broken” – that is, the bottom half was removed so that her crotch was now at the bottom edge of the fore-shortened table. Next one of the nurses would stand between the mother’s wide spread legs and pull her hips down until her buttocks were literally hanging off the table over thin air. The reason for this unusual position was to take the weight off the back of the mother’s pelvis and help overcome the detrimental effects of putting her in the lithotomy position.
This reflected a very astute understanding of the childbearing pelvis by the obstetricians of yester year. The large triangle shaped bone at the base of the spine – the sacrum and its smaller appendage known as the coccyx – is attached to the end of the spine with a hinge-type joint. In normal circumstances, this hinge is in the neutral position and these bones curve slight inward and encroach on the “birth canal”.
The “birth canal” is not an anatomical structure but instead refers to a temporary combination of the vagina and the dynamics of the baby moving through it and out of it into the world. It is a potential space that is a result of the hormones of pregnancy and the birth process itself.
The hormones of pregnancy makes the ligaments that hold the bony pelvic plates together become stretchy so that the weight of the baby actually helps to press these bones slightly apart, making more room for the baby to pass. The spring-loaded hinge of the sacrum (with coccyx attached) permits this big bone plate to naturally move out of the way as the baby is pushed through the birth canal. The mechanics of this is similar to how the family dog or cat can push open a small pet doors with its head.
The combination of ‘right use of gravity’ (mother who is upright and mobile) and sacral mobility can add as much as 2.5 centimeters (about an inch) to the pelvic outlet. This is often the difference between a baby that fits (i.e., a natural vaginal birth) and one that results in the medical diagnosis of “cephalo-pelvic disproportion”, which requires forceps or a cesarean to rescue the baby from this man-made problem.
Tag-edit Sept 04, 2013
A fully dilated cervix equates to an open channel between the uterus and the upper end of the birth canal. This is the technical beginning of the second stage of labor, in which the baby’s head is propelled out of the uterus and down into the vagina by the contracted uterus acting as a piston in combination with the voluntary pushing efforts of the mother as she uses her abdominal muscles to assist the uterine effort. As the baby’s head extends further and further down into the vagina, a centimeter at a time, its continued progress depends on adequate space between the pubic bone in the front and the sacrum in the back. Except for women with a huge pelvis or a tiny baby, the adequacy of the birth canal is dependent on the mother’s relationship to gravity and whether or not she is bearing her weight on her sacrum.
Unfortunately weight-bearing on the sacrum prevents the normal hinge action because there is no place for the sacrum to be displaced – the mattress is in the way. To prevent this “mattress dystocia, the unconscious woman’s hips were pulled so far down on the table that her butt literally hung off the table, in recognition of the benefits of sacral mobility. While the lithotomy position was anti-gravitational and in other ways contributed to fetal distress and other forms of pelvic dystocia, this novel approach circumvented at least one of the problems of lying supine, as it permitted the sacrum to be moved from the inside as the baby’s head and body passed by.
In the continuing surgical preparation of the mother for delivery, the next step was to spray-painted her crotch with Mercurochrome. Then her legs and lower body were hidden away under several sterile sheets. When 50 cents worth of caput was visible (able to see about 3 centimeters baby’s head as it stretches opens the birth canal), the nurse anesthetist put the mother to sleep with general anesthesia. Anesthetizing the mother usually interfered with or even stopped her voluntary pushing efforts, which helped delay the birth until the doctor got there.
The patient’s doctor or the OB resident were already been notified by then and usually arrived about this time. He (OB doctors were 99% male) gowned up, scrubbed her perineum again with antiseptic solution, emptied her bladder with a rubber catheter and then cut a ‘generous’ episiotomy to protect her pelvic floor from the trauma of birth (!) and to facilitate the routine use of “outlet” forceps.
The purpose of using forceps routinely was both to “spare” the mother’s perineum from the trauma of normal birth (!) and to keep the doctor well practiced so that when forceps were actually necessary, he would be appropriately skilled. A third reason, as mentioned above, was that anesthesia seriously curtained or even obliterated the mother’s voluntary pushing efforts. Forceps became necessary under the effect of drugs and anesthesia which, in a convoluted way, were also used to time and control the spontaneous events of labor and birth, so as to better manage the time of obstetricians. It was a seamless system carefully orchestrated to work beautifully for doctors and hospitals
For the doctor, part of the birth drama was to carefully ponder which of the half-dozen type of forceps was right for the job – Simpsons, short handled Elliots, McCleans, long-handled Pipers for the after coming head of a breech baby, etc. It was the job of the nurse to find the requested pair in the delivery room cabinets. After unwrapping them from their sterile package, she dropped them with a muffled bang on the sterile-draped instrument table.
This was a strangely hypnotic activity, the shiny metal gleaming in the bright beam of the overhead OR light and the nurse so “professionally competent” in this special role of helper, garbed in surgical scrubs, operating room cap and mask – it was dramatic like being in a Hollywood movie. Because forceps were so central to the delivery, it seemed that it was these instruments in combination with the obstetrician’s surgical skills, and not the mother, who made the miracle of birth possible.
Before being used, the forceps blades were dipped in a red antiseptic soap called “Septasol”, to make them slippery and then slid one blade at a time up into the unconscious mother’s vagina. The heavy handles, which protruded from the mother’s vagina by 10 to 12 inches, were locked together and left hanging there for a while. Often bleeding from the gapping episiotomy would produce a small river of bright red blood which made a hollow ringing sound as the stream splashed against the bottom of the stainless steel bucket on the floor underneath the mother’s buttocks. To proceed with the delivery, the doctor pulled steadily on the handles of the forceps until the baby’s head emerged and then the protocol was revered, the forceps blades unlocked and removed one at a time.
As soon as the anterior shoulder of the baby could be seen at the top of the mother’s birth canal, the delivery room nurse would be instructed to give the mother an intramuscular injection of the anti-hemorrhagic drugs “Pitocin” and “Methergine”. This routine was to prevent (it was hoped) excessive bleeding after the birth or postpartum hemorrhage, a life-threatening type of bleeding.
A common aspect of delivering a woman under general anesthesia was fundal pressure applied by the nurse in coordination with the doctor’s efforts to pull from below, especially for the delivery of the shoulders. The nurse would stand on a step stool at the midway point of the delivery table, learn across the mother’s body and grab the handle on the far side of the delivery table while pressing the long bone of her forearm down laterally across the mother’s abdomen, at the top margin of the uterus. Her other hand, the one closer to the mother’s head, was used like a piston to help force the original arm downward on the uterus in a T-bone configuration. It was hoped that this fundal pressure by the nurse would push the baby down and out from above.
Sometimes this forceful pushing on the mother’s mid-section, right over her stomach, caused the mother to vomit. Because she was unconscious from anesthesia which obliterated her normal gag reflex, women sometimes aspirated stomach contents, causing a fatal pneumonia. This was one of the reasons that mothers were not permitted to eat or drink in labor. We never considered the alternative – to refrain from doing this rather violent maneuver in the first place and instead use gravity to assist the spontaneous birth of the baby. Other complications of using fundal pressure on anesthetized women was uterine rupture and impacting the shoulder of the baby, causing shoulder dystocia and perhaps contributing to Erb’s palsy, a permanent nerve damage that caused the baby’s arm to hang limp and useless at its side.
After the baby was delivered, it was held upside down while the doctor suctioned its throat deeply with a bulb syringe and then immediately clamped and cut the umbilical cord, all in about 20 seconds. At that time it was believed that the blood circulating in the baby’s cord (2 or3 ounces of rich stem cells, the equivalent of 2 pints of blood in an adults body) was bad for the baby – that it was the cause of what we now know is the normal ‘physiological’ jaundice of the newborn. Contemporary research has identified that for premature babies and term infants suffering from respiratory depression or possible meconium aspiration, the loss of this “2 pints” is a further insult to an already fragile system. (citation here)
Unfortunately, babies born to narcotized, anesthetized mothers and delivered via forceps were predictably depressed (and always deprived of a crucial part of their blood supply). It was one of my jobs as an L&D nurse to “fluff” up the baby with positive pressure O2 and other methods to stimulate it and attempt to trigger spontaneous respirations.
About 20% of the babies were severely depressed and some of them (maybe 1%) just never did breathe, despite our best efforts at resuscitation. When that happened we were so glad that the mother was unconscious so we didn’t have to face her grief over the stillbirth of her baby and our failure to prevent such things. Doctors and nurses rarely connected the drugged and anesthetized status of the mother and the respiratory depressed baby in any useful ‘cause and effect’ relationship, in spite of the many warning carried in package inserts and obstetrical textbooks on the respiratory depressing effects on the neonate of drugs and anesthesia. However, I have always believed that at some subconscious level we did understand the detrimental effects of our actions, the guilt of of which contributed to the general craziness of obstetrical nursing and obstetrical practice.
While the nurses were focused on resuscitating the newborn baby, the physician reached deep into the mother’s body with his gloved hand and lower 4 inches of his arm, through her vagina and up into her uterus to manually separate the placenta from the wall of the uterus. The 8-inch round, one inch thick placenta was then folded into a round blob about the size of large grapefruit, pulled out in the doctor’s hand and discarded in another stainless steel basin.
The final act of the delivery room drama was when the doctors sutured the perineal incision, often chatting casually or making jokes about what the he described as the “husband stitch”, a little extra service he provided to her husband by doing his best to sew her up tight and thus return her vagina to the “virginal” status of someone who had never given birth. The comment was that otherwise the husband would complain that after his wife had a baby, having sex with her was “like walking into a warm room”
The newly delivered mother lay on the stretcher that we used to move her from the delivery room for several hours, until she was conscious again. In the mean time she often vomited repeatedly while coming out from under the effect of the general anesthesia. Every 15 minutes for two hours one of the nurses would peek between the mother’s legs to monitor her bleeding and poked and prodded her tender uterus by mashing down hard enough for the mother to yell out in pain and try to grab the nurse’s wrist to stop her. After the mother was fully awake we provided a bedpan for her to pee and failing that, catheterized her – a painful procedure for a newly postpartum women with stitches.
Finally the tortured woman was awake enough to be taken by gurney to the nursery, where one of the nurses would hold her baby up for the new mother to see for maybe 30 seconds (if the nurses weren’t too busy). They she was finally put to bed on the postpartum floor, where she would stay for the better part of a week. After 24 hours her baby would be brought to her every 4 hours during the day, but babies were bottle-fed in the nursery at night because (obviously), new mother really needed their sleep.
I now refer to this massively interventive style of obstetrical care as “vaginal Cesarean”. However, our vaginal birth rate was 97% and our actual Cesarean section rate was only 3%.
