Last edited 05-16-2023 @ 9 am
Part 1-C: Dr. JWW’s invention of elective hospitalization of healthy childbearing women to generate revenue for upgrading and equipping general hospitals
 How Dr. J. Whitridge’s Williams’ big dream got started
How Dr. J. Whitridge’s Williams’ big dream got started
Dr. Williams’ big dream was the result of several remarkable experiences over the course of several decades that lead to insights about the American system of hospitals. The first of these insights began after his graduated from medical school in 1888, when he sailed to Europe to take clinical training in the biggest and best hospitals of on the European continent.
At that time, there was little to no clinical training available in American medical schools — just two years of didactic education in anatomy, physiology, chemistry, and formulation of medicinal preparations (i.e. drugs) from chemicals and other substances.
Clinical Training in medical school ~ the “new kid” on the block
In the late 1800s, the idea of clinical training — internships and residency programs — had not yet been integrated into medical schools the United States. Of th 8,000 or so hospitals in America, all but about two dozen were very small (2-to-10 bed) private, doctor-owned facilities housed in an aging mansion, similar to the private hospital in the Downton Abbey series. The daily patient census of these tiny hospitals wasn’t large enough to provide enough ‘teaching cases’ for the clinical or “hands-on” training of medical students.
How Dr. JWW came to be a “visionary” in establishing a nationwide system of general hospitals in the US
Dr. JWW was fourth generation son from a wealthy family of doctors and lawyers originally from England. His father was a physician and his mother, Mary Whitridge, also came from a distinguished medical family. After graduating from medical school, he was able to hop on an ocean liner and head for Europe, where he studied bacteriology and pathology at universities in Berlin, Vienna, Leipzig, Prague and Paris from 1888 to 1893.
That was when Dr. JWW was hired by brand new Johns Hopkins University Hospital and appointed Associate Professor of Midwifery. However, in 1894–1895 he want back to Europe, this time to study obstetrics and pathology. When he came back to Johns Hopkins he was promoted to a professor in obstetrics for the University, and “Obstetrician‐in‐chief” to the hospital.
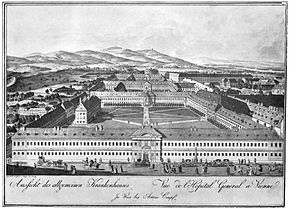
He was struck by how remarkably different hospitals in Europe were, both size and function, than those in United States. In addition, Europe had a national system of regional “general” hospitals. These were enormous institutions able to treat any type of medical, surgical, obstetrical, pediatric problem, as well as any a major emergency. At the same time, they functioned as centers for the clinical training of medical students.
Dr.Williams was very impressed with the quality and quantity of medical services available to the general population of these countries. He was also excited about the opportunities for clinical training these big hospitals provided to medical school student and graduate students like himself and acutely aware the US had nothing that compared.
Upon his returned to America, he was shocked by just how inadequate our tiny one-room hospitals were when compared to the quality and quantity of medical and surgical services provided by Europe’s big regional hospitals. He was also burdened by the knowledge that the small town doctors who owned and ran these one-room hospitals in the US would never be able to match the sophisticated and high-quality care available in the European system.
At the same time, 98% of American hospital were the equivalent of a medical hotel with amenities such as room service and nurses to change bandages and help patients to the bathroom. They were the dying embers of the pre-scientific practice of medicine which mostly consisted of “palliative care”.
Historically, medical practice was founded on the personal “therapeutic relationship” between a medical doctor and his patients. If on was lucky, the doctor was a reassuring presence that took the patient’s hand. entoned encouraging words and the hope that patient would eventually get well. Thousands years of medical impotence was abruptly rendered obsolete during next few generations as new scientific leaps of modern medical knowledge forever foreclosed on us as helpless victims of a cruel Fate.
This began in 1865, when Sir Joseph Lister, royal surgeon to Queen Victoria, developed and implemented the general principles of asepsis and the particular idea of ‘sterile technique’ to be used during surgical operations. This was largely based on the unpublished work of Louis Pasteur, who discovered the Germ Theory of contagion and infectious disease in the 1860s, but these extraordinarily important ideas were not published and accepted by the international community of scientists and physicians until 1881.
 Many other scientific discoveries in the area of medicine followed, one of the most important being the discovery of radium and harnessing of ‘x-rays’ in 1895 into a machine that allowed doctors to see inside living people for the first time.
Many other scientific discoveries in the area of medicine followed, one of the most important being the discovery of radium and harnessing of ‘x-rays’ in 1895 into a machine that allowed doctors to see inside living people for the first time.
Now it was up to the next generation — the grandsons — to implement all this at the practical level by making scientifically-based medical care available to the ill and injured in ‘modern’ general hospitals. And as noted earlier, modern medicine was capital intensive and thus, very expensive.
How best to implement these important insights?
Dr. Williams simply wanted to make modern ability to diagnose and treat serious injuries and illnesses and effectively cure previously fatal diseases available to the rest of the country via the trifecta of modern medical science — advanced understanding of the human biology, trained professionals. and use of modern technologies.
What was needed to fix the problem was crystal clear to Dr. Williams. America needed to replace the thousands of old-fashion 2-10 bed 19th-century hospitals with a modern nationwide system of full-service hospitals that were able to provide comprehensive medical and surgical services to the general public, as well as providing round-the-clock emergency services.
Dr. Willams’ personal goal was to make these state-of-the-art institutions the new standard of care, available from sea to shining sea. He envisioned at least one of these facilities in every town of 3,000 or more, and looked forward to the day when they become as “uniform, if not quite as abundant, as schoolhouses and libraries“.
Definition of a 20th-century General Hospital: The services of a general hospital are available to the public, irrespective of ability to pay and provides care across the entire spectrum of health-related needs for all age groups and all conditions.
It also has emergency services immediately available to anyone with an acute illness or life-threatening injury. It is staffed 24-7 and fully-equipped with relevant supplies, medical equipment, and scientific technology of the era, such as x-ray machines, microscopes, and ‘state-of-the-art’ operating room and good lighting.
This also includes the vital support services for any acute-care medical facility — a hospital kitchen and laundry and the all-important central supply department to purchase and stock necessary medical supplies and autoclaves to sterilize equipment and surgical instruments.
This already was the standard in European countries, but when Dr. Williams was writing his book in 1914, the United States had yet to develop a comparable system and was still 200 years behind the curve. Not only was there a general failure of imagination (neither doctors nor patients knew just how much was missing from the system of medical care), but even those who recognized the enormous advantage to everyone in the entire country were stopped cold by a single word — MONEY — that is, the lack of funding.
The Big Brick Wall that couldn’t be reasoned with, hollowed out, broken thru, tunneled under or gone around!
The biggest financial stumbling block in the US was organized medicine. Since the inception of the AMA in 1847, the organization has always been fiercely opposed to any ‘meddling’ by the government in the provision of medical services or the running of hospitals.
This was in large part a reaction to and rejection of the European system of nationalized hospitals. From a physician’s perspective, that system was the public equivalent of our modern-day VA hospital system, that is, is funded by the federal government, with medical services provided at the local level by salaried physicians who are in the employ of the federal government.

Historically preserved building that was originally a small private hospital owned and run by a much-admired local doctor
However, doctors saw the practice of medicine very differently. They believed it was and should stay a small business and their relationship to this ‘free market’ was that of plucky entrepreneurs. It was as natural for a medical doctor to expand his medical practice by opening a clinic or small hospital in an older mansion (picture scenes from “Downton Abby”) as it was for a farmer to open a roadside fruit and vegetable stand and eventually find himself running a busy chain of grocery stores.
The Wild West — not just for Wyoming cowboys but a way of thinking about the American free-market
Organized medicine considered any attempt by the government to use public tax money to build hospitals and to hire doctors as salaried employees to run them to be “socialized medicine”, which was the worst kind of insult. American doctors considered all aspect of medical practice to be their private property/business opportunity, to do with as they pleased. They were fiercely against the nationalized systems in Europe, which they believed violated the economic ideal of our free enterprise system and the bureaucratic management of such bigger nationalized facilities interfered in the sacred “doctor-patient relationship”.
The idea here is that the doctor’s loyalty, motivations, and contractual obligations would first go to whoever was paying the bill for his services. As an employee, that would mean “the system”, which theoretically killed off his motivation to do ‘better’, to innovate, work harder, etc. since none of these professional qualities would translate into a bigger paycheck.
The AMA line also claimed that ‘socialized medicine’ was a real disservice to patients. The particular issue was decision-making control over the patient’s treatment: Who decides what is ‘best’ — her own doctor or would he be ‘second-guessed’ by his supervisor or be forced to follow the hospital’s policies and protocols? These two factors are the core of the sacred “doctor-patient relationship” as it was (and is) seen by the AMA.
In general, the strong opinion of organized medicine in 1914 was that doctors were professionals, which meant being their own boss. It was an insult to one’s professional status to become a ‘mere’ employee and have to work under someone else’s supervision and be bossed around. Due to their superior medical education, a doctor’s role was to boss other people around — just ask the nursing staff of any hospital!
Bottom line, virtually everything about socialized medicine was so deeply repugnant to doctors that they were willing to fight to the death. At a practical level, this was achieved by paying their membership dues to the AMA and depending on the organization’s crack lawyers and PR experts to stave off any “well-meaning” but nonetheless incremental encroachments on their freedoms.
During this period of time, the unquestioned, unbreachable political influence exerted by the AMA on politicians of that era (1850 to 1990s) equaled, if not exceeded, the influence currently exerted and ‘enjoyed’ by the NRA had in relation to its total embargo of any effective action to improve gun safety in the US.
Both ‘movements’ share the characteristic of having become a quasi-religious belief; one is either “with us or against us” in an emotion-centric stance that logic plays no part in. This allows it’s adherents to vilified their oppositions as treasonous and treacherous infidels. However, at the bottom of this quasi-religious fervor by both organized medicine and the NRA’s organized resistance to sane gun laws is the very same “follow the money” dynamic.
Whether it is profiteering hospitals or greedy gun manufacturers, once such a money machine has been fired up and starts pumping out cold cash, it’s perpetuation trumps every other ethical or social consideration. Like a religious belief, it becomes an obsession, and soon thereafter, a hopeless helpless addiction in which the sufferer is forever locked in his or her irrational mind, impervious to the reach of reason or any form of common sense.
It was not lost on Dr. Williams that the AMA’s reiteration of Patrick Henery’s famous diatribe: “give me liberty or give me death” didn’t mean that doctors actually were willing to die for their cause, but that ordinary Americans who couldn’t afford to pay for proprietary medical services would die as a result.
Even worse, Doctor Williams knew full well these deaths could be prevented by timely access to state-of-the-art medical services. He knew this because comprehensive medical care was already available publicly to those living in the Baltimore area by his very own employer – Johns Hopkins University Hospital. This was the model of medical care that he believed should be accessible everywhere in the country as it was already available in Western Europe.
Lacking a public tax-supported national system as existed in many parts of Europe, the technologically-rich hospital business in the US was forced to look to their patients, which by definition are people that are sick, injured, infected w/ communicable diseases like TB or suffering an acute mental breakdown. It became increasingly clear that hospitals could no more depend on the seriously ill or injured to pay for their medical care than we can expect school children can pay their teachers’ salaries or prison inmates to reimburse their jailers for the cost of their incarceration. In fact, we don’t even ask people who borrow libraries book to pay a hefty charge for the privilege.
The conclusion was inescapable to Dr. Williams: Without a public tax base, there were just not enough sick people (as paying customers) to support 20th century ‘modern’ medicine. The apparently insurmountable problem was money — how to finance a nation-wide system of general hospitals without public funds?
The big paradigm shift for American Medicine ~ inventing the economic engine for private profit-making hospitals
Despite the intense need and given the resistance by organized medicine to federal money and predictable blocking of any attempt to work out some kind of public-private partnership, there was just no obvious way to underwrite a national hospital system.
In the first part of the 20th century, the typical acute-care hospital patient was gravely ill or injured and might linger in the hospital for weeks or months, in need of intensive, expensive care that often they were unable to pay for. Dependent as hospitals were on sick people as paying customers, the traditional business model of American hospitals was often drowning in its own red ink.
It was obvious to everyone in the inner circle that hospitals themselves would never be able to pay for their own transformation — the paradigm jump from their grandfathers’ 19th pre-scientific hotels to the post-science era of hospitals as the modern font of all medical miracles.
 But Dr. Williams was both undaunted and determined. History doesn’t tell us if the idea came to him like a lightning bolt out of the blue or snuck up quietly on soft cat paws in the middle of the night.
But Dr. Williams was both undaunted and determined. History doesn’t tell us if the idea came to him like a lightning bolt out of the blue or snuck up quietly on soft cat paws in the middle of the night.
Whichever it was, there was a moment of inspiration when Dr. J. Whitridge Williams invented a brand new economic model for running hospitals as a profitable business. This also simultaneously created the pot of gold that would finance his dream for a national system of well-staffed and fully-equipped general hospitals – one for every community with a population of 3,000 souls or more.
The lynchpin of Dr. JWW’s business plan was pure genius – a truly innovative idea for a newly expanded and profitable market for hospital services. The secret sauce was to electively hospitalized healthy patients as paying customers, specifically, the million-plus healthy middle and upper-class childbearing women that gave birth every year in the US.
Dr. J. Whitridge Williams’ new model would, for the first time in the history of American hospitals, be able to provide them with a dependable and profitable revenue stream by dramatically expanding ratio of profit-generating patients to non-paying sick people, thus turning hospitals into profit-making businesses. However, Dr. JWW’s plan, with its ambitious goals, also had many ‘moving part’ and would require a number of coordinated and interlocking phases that would take several decades to play out.
Continue to Part 1-D ~ Selling his odd ideas about childbirth to the public and philanthropists
Word Count: 2,400