2006 San Francisco SU Conference ~ Part Two:
 Chain of Inevitability ~ The beginning of obstetrics in America as a surgical speciality resulted in the medicalization of normal childbirth. This ended of the non-medical management of normal childbirth as a services provided by the obstetrical profession.
Chain of Inevitability ~ The beginning of obstetrics in America as a surgical speciality resulted in the medicalization of normal childbirth. This ended of the non-medical management of normal childbirth as a services provided by the obstetrical profession.
Hospital-based obstetrics both replaced and displaced the profession of midwifery, which meant that non-interventive support for normal labor and spontaneous birth, in which women were primary birth attendants, was no longer an available options for women giving birth in American hospitals
Faith Gibson, LM, CPM
 Our modern system of medical education was developed long ago in Europe , during the historical Age of Enlightenment. The earliest origins of modern obstetrics began in the 1600s as a part of the newly emerging profession of scientific medicine.
Our modern system of medical education was developed long ago in Europe , during the historical Age of Enlightenment. The earliest origins of modern obstetrics began in the 1600s as a part of the newly emerging profession of scientific medicine.
For most of its history, medicine was not a science – that is, it wasn’t an applied scientific discipline. The scientific method is usually defined as the rigorous and unbiased investigation of phenomenon thru repeatable experiments. This is accompanied by the formal publication, peer review and dissemination of new knowledge to the wider scientific community. Universal adoption of these principles within the medical profession didn’t even start until the 17th century C.E. and required many more centuries to become what we now call ‘modern medicine’.
To begin with, doctors had little or no understanding of physical anatomy, physiology or the contagious nature of infection. In the 17th century, study of the human body and the pathology of disease did not yet include the scientific knowledge obtained through dissection of human cadavers. It wasn’t until 1881 that the existence of microscopic pathogens — what we now call bacteria or the ‘germ theory of disease” — was identified as the origin of infection and contagious illness.
In the 18th and 19th century, the most dramatic and important advance in medical education was the addition of clinical or ‘bedside’ teaching as a crucial part of medical training. This resulted in the use of hospitals as clinical learning labs. The earliest hospitals arose during the Middle Ages as charity hostels run by Catholic nuns to house the indigent. They were the perfect place for medical schools to teach students, as they provided a steady stream of ill and injured as teaching cases or ‘clinical material’.
Long before Henry Ford applied assembly line methods to auto manufacturing, the medical profession had figured out how to create an institutional environment that would maximize the goals of medical education. Hospitals evolved into places for both teaching and treatment and by the 16th century were organized around the needs of medical education. Street people who were sick became teaching cases for medical students, receiving free treatment in exchange for room and board. For the first time in history, medical students had the opportunity to learn anatomy by examining the living and dissecting the dead and to study disease by performing postmortem autopsies. These activities were absolutely crucial steps in the march towards modern medicine as an applied science as we know it today.
However, as late as the 1700s, doctors in most parts of Europe were not permitted to be present during childbirth. It was thought to be immodest and sinful and was punishable in some countries by death. Despite such strong disincentives, a few particularly brave doctors worked to expand obstetrical knowledge. This included the invention of obstetrical forceps and other rescue operations that midwives were not able to do.
Eventually the disciple of medicine evolved into a university-trained ‘profession’. Its graduates ‘professed’ to a strict code of ethics (the origin of the word ‘profession’) that was approved by the state Church. This accorded doctors a special status, absolving them from the traditional bounds of modesty. They were permitted to study female reproduction and to finally provide obstetrical interventions when the art of the midwife failed.
Ten Slippery Steps
Problem # One ~ the 19th century
By the end of the 1700s, many physicians were providing routine “midwifery” care – the official term for non-surgical maternity care as provided by either doctors or midwives. Medical education included training in normal midwifery and in operative obstetrics. This required a steady stream of pregnant patients so that students could acquire the necessary medical knowledge and technical skills. At the time, childbearing women were normally attended in their own homes by midwives and doctors. This one-by-one type of care could not provide the necessary clinical experience required to educate a whole class of medical students.
Fix #1 ~ 1800s: In order to meet the needs of obstetrical education, normal birth had to be institutionalized. Charity hospitals already offered ‘hospitality’ to destitute and homeless pregnant women, including prostitutes living on the street. During the last months of pregnancy they were housed in these early hospitals and cared for by midwives during labor and birth. Medical educators turned this pool of institutionalized women into a steady stream of clinical material for students of obstetrical medicine.
Medical students were required to perform physically invasive, frequently repeated pelvic exams on laboring women in order to learn about the biology and physiology of normal labor. The student’s need to acquire clinical skills and manual dexterity was also associated with the liberal use of medical and surgical interventions. Students learned about the pathology of female reproduction by performing autopsies on pregnant women or those who died during or after giving birth.
However, all of this was happening a hundred years before anyone understood the germ theory of infection and long before the invention of sterile exam gloves. Without disinfecting their hands, medical students went from the dissecting room, where they had just performed autopsies on patients who died of hospital acquired infections, to the labor wards. Then they went from bed to bed doing internal exams, unintentionally spreading the germs of a lethal infection to all the women in labor that day.
Problem #2 ~ 1830: Through out human history, a tiny fraction of childbearing women became ill after birth with a potentially fatal infection commonly called ‘childbed fever’. But this was a rare and isolated event. However, the assembly line process associated with obstetrical education turned those statistics on their head and made the exception into the rule. Physicians recognized early on that aggregating childbearing women together in an institutional setting resulted in a drastic increase in maternal and infant mortality. They also observed that indigent women who gave birth on the doorsteps of the hospital, prior to admission to the maternity wards, were remarkably free from infection, as were their newborn babies. But nobody understood why.
Regrettably, cultural ignorance of the germ theory and the many invasive practices associated with training medical students resulted in institutional epidemics of childbed fever or ‘septicemia’. Five to 50 percent of women and babies who delivered in these charity hospitals died. The local population began to associate hospital childbirth with dying.
The medical profession’s attempt to understand and perfect childbirth was haunted by an ever increasing rate of maternal and infant mortality. In order to better understand what was killing these healthy women, the best teaching institution insisted that post-mortem dissections be performed on every woman who died from puerperal sepsis. But despite these heroic efforts, the deaths went on unabated. Quite unintentionally the medical profession itself had become the vector for these fatal infections. Obstetrical educators did not realize it, but the care being provided for normal birth was actually based on the artificial needs of medical education instead of the normal biology of childbirth. This system also did not acknowledge the physical, psychological and social needs of the mother. Concentrating laboring women together in an institution exposed healthy women to contaminated bedding and other environmental sources of infection. The routine use of invasive pelvic exams in the absence of aseptic technique and sterile supplies systemized the spread of infection and institutionalized iatrogenic mortality. Routine use of practices that were central to the educational process but had never before been a part of normal birth resulted in hospital-based epidemics of childbed fever.
The 1830s Fix:
Concentrating thousands of childbearing women in contaminated and highly contagious hospital environments caused problems that doctors didn’t understand. In general, obstetrical professors confused cause and effect. To them, ‘more’ was ‘better’. They were convinced that only better training for medical students could bring an end to these vexing problems. During the 1830s the imagination of obstetrical educators was captured by a new, cutting-edge idea — the use of cadavers to teach manual dexterity skills. It was assumed that these improved abilities would reduce the mortality rate of their patients, perhaps by preventing a long labor through the adroit use of forceps.
At the beginning of the 19th century most teaching hospital depended on a sophisticated teaching manikin developed about a 100 years before by the French midwife to King Louis the XV. These life-size teaching dolls each had an anatomically correct pelvis, pregnant uterus occupied by a realistic fetal doll, amniotic fluid, a placenta and umbilical cord and access to the pregnant uterus thru a working genital tract. This biologically safe teaching devise was used to teach midwifery skills to student midwives and instrumental and manipulative obstetrics to physicians and medical students.
However, as dissection became an increasingly important part of medical school education, the obstetrical manikin fell out of favor all across Europe . Gradually the bio-safe manikin was replaced by the bio-hazardous cadavers of women who died in childbirth, with the assumption that such cadavers were a “superior” teaching resource that would result in a superior medical education. Each body to be used for teaching purposes was specially prepared by dissecting out the abdominal organs and then placing a recently deceased baby inside the pelvic cavity. By passing a series of newborn cadavers down thru the pelvis of a recently deceased childbearing woman, a professor of obstetrics could control the learning experience and assist his medical students to could carry out vaginal exams, determine fetal lie and position, apply obstetrical forceps, practice fetal destructive operations and learn life-saving maneuvers such as podalic version for obstructed births. Technically speaking, this was a successful educational strategy.
Modern-Day Examples of Bio-safe Obstetrical Teaching Manikin  |
|
| Obstetrical Manikin – This is an anatomically correct pelvic model with full term newborn and placenta to give realistic practice in multiple techniques.
The Simulator is designed to facilitate demonstration and practice of palpating the internal birthing canal. The simulator clearly shows the relationship between the fetal head and the ischial spines of the pelvic bone of the mother during the birth process. The realism of the simulator will help students bridge the gap from classroom to bedside. |
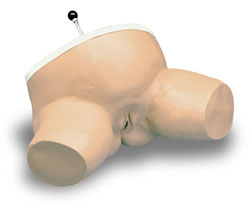 |
| The simulator is designed to highlight the ischial spines which are of great obstetrical importance. The line drawn between the ischial spines typically represents the shortest diameter of the pelvic cavity. The ischial spines can be readily felt during a vaginal examination, and serve as valuable landmarks in ascertaining the level to which the presenting part of the fetus has descended into the pelvis. | The Simulator features a fetal head which will lock in any one of three lock stations. Minus Two Station shows the position of the fetal head when it lies above the ischial spines. Zero Station shows the fetal head directly between the ischial spines. Plus Three Station shows the fetal head below the ischial spines ready to enter into the birthing canal. One-year warranty. |
Problem #3 ~ 1840s: However, the use of cadavers for teaching virtually guaranteed that highly-contaminated organic material would be carried into the labor wards on the hands of medical students. At the university hospital in Vienna , as elsewhere in Europe , teaching cadavers made an already bad situation worse. Even more undelivered mothers became contaminated with the haemolytic streptococcal bacteria and developed a virulent septicemia that caused death within 72 hours. Out of 3,000 deliveries annually, 700 died each year — two or more mothers and babies each and every day.
The 1840s Fix ~
At the university hospital in Vienna , an associate professor of ‘midwifery’ — Dr. Joseph Semmelweis — began to question many of the common practices used by the obstetrical staff and students. He was convinced that something they were doing in Division One of the hospital was responsible for the mounting maternity mortality rate among obstetrical patients. It was common knowledge that the infection rate of women who delivered in the midwifery part of the hospital (Division Two) or gave birth at home, was only a fraction of the rate for Division One. Dr. Semmelweis employed the true spirit of scientific investigation and eventually identified the iatrogenic nature of childbed fever. In his own words Dr. Semmelweis concluded that: “puerperal fever is caused by the examining physician himself, by the manual introduction of cadaveric particles into bruised genitalia”.
History records that Dr. Semmelweis reformed these iatrogenic practices by introducing prophylactic hand washing in chlorine of lime solution. Like a sudden overnight miracle, maternal deaths in his institution fell from 18.27% to 0.19% in the eight months between April and December of 1847. As a result he devoted his entire career to preventing unnecessary maternal deaths by teaching and preaching the use of aseptic principles. Unfortunately, these ‘radical’ life-saving ideas were ridiculed and dismissed as absurd by other doctors. Doctors thought it inconceivable that the healing hands a physician (or his instruments) could ever, under any circumstances, be a vector for a contagious fatal illness. For his trouble Dr. Semmelweis soon lost his prestigious post in Vienna ’s most famous hospital, lost his reputation and eventually his profession. He died shortly afterwards leaving a wife and several young children.
Problem # 4 ~ the 1880s: Dr. Semmelweis’ simple but effective solution was ignored by his contemporaries, who could not wrap their minds around something so unglamorous and straightforward as hand washing. As a result, education-based obstetrical practices continued on unexamined and unabated, as did the high level of maternal mortality associated with hospital delivery. However, there was growing criticism of this system.
A small number of astute physicians all over the world, including our own Oliver Wendell Holmes in Boston , studied childbed fever. They observed that the repeated virulent epidemics of puerperal sepsis were virtually absent in places that midwives (who did not use instruments) managed normal birth instead of doctors (who did) and where autopsies or dissections were not being done by the same practitioners who attended deliveries. Over the course of a hundred years, many doctors had publicly identified the iatrogenic nature of these childbirth infections. An article by Oliver Wendell Holmes published in the New England Journal of Medicine and Surgery in 1843, entitled ‘The Contagiousness of Puerperal Fever’. In identifying the contagious nature of birth-related septicemia, Oliver Wendell Holmes agreed with other researchers that the disease was often transmitted, via an unknown agent, by both physicians and nurses.
In regard to epidemic levels of maternal-infant mortality from infection, obstetricians also had discussions among themselves on the vastly higher death rate for hospital births versus “private practice” (women attended in their own homes). A renowned professor of obstetrics from Edinburgh, Scotland lamented in 1881 that in his institution: “…maternal deaths during childbed – by which is meant death occurring within four weeks after delivery — have been shown to be striking in their frequency” “The present Maternity Hospital, being a necessity, and puerperal fever having been shown to exist there, [is known] to have been the direct cause of death in 1 out of every 32 women …. ”
Despite the high mortality associated with the hospitalization of maternity patients, the conclusion by medical professionals was that hospital birth was an absolute necessity. It was only place to house indigent pregnant women and, even more important, medical educators concluded that the high quality of clinical instruction vital to medical education could only be provided in a hospital environment.
The Fix ~ 1881: It was not until 1881 that a French physician, the now famous Dr. Louis Pasteur, established the central role of microbes — commonly known as ‘germs’ or ‘pathogens’– in causing illness and infection. On a chalk board at a prestigious medical meeting Dr. Pasteur drew a graphic representation of what the streptococcus bacteria looked like under a microscope — rectangular microbes that resembled a string of box cars on a train track — and said “This, gentlemen, is the cause of Childbed Fever”. With this discovery, Dr. Pasteur delivered the fatal blow to the erroneous theory ‘spontaneous generation’ – a dangerous doctrine that for the previous 2000 years insisted that life could arise spontaneously in organic material.
In order to preserve hospital birth as an educational necessity and eliminate iatrogenic cases of childbed fever, the obstetrical profession threw itself into the development of new aseptic practices for maternity care. First and foremost was to forbid the performance of autopsies and dissections in the same building and by the same practitioners as attended cases of childbirth. Other changes included the forced bathing and pubic shaving of women on admission to the labor ward (in case they had bed bugs or pubic lice!), as well as meticulous attention by the housekeeping department to disinfecting bed linens. In the 1880s, the contagious nature of hospital birth focused particularly on aseptic techniques used during the immediate postpartum. Doctors believed that the birth and the first 24 hours was the period of greatest vulnerability.
Recommended aseptic techniques included scrupulous hand washing as well as a procedure called ‘panning’ that continued to be used in American hospitals until the 1960s. Panning consisted of placing the newly delivered woman over a sterile bedpan in order to wash the mother’s labia and perineum with a series of sterile cotton balls wet with antiseptic soap. It required the use of a special pair of sterile of tongs so that the mother’s body was never touched by the nurse’s fingers. This was done every four hours as well as every time the mother needed to urinate or change her perineal pads (i.e. ‘Kotex’ napkins). This procedure was thought to be absolutely vital to the prevention of infection. However, the 1880s version of panning was followed by the very unpleasant practice of soaking perineal pads in a strong antiseptic solution. These wet pads were then put on newly delivered mothers for the first 24 hours. This must have been horribly uncomfortable and not actually very sanitary.
Debunking the idea of ‘spontaneous regeneration’ and replacing it with the germ theory is what ushered in the real beginning of what we now call “Modern Medicine” as an applied science. This scientific understanding of microbiology and the improved antiseptic practices really did dramatically lower the maternal mortality rates. However, the story of iatrogenesis was not yet over. Concentrating large numbers of childbearing women in hospitals still resulted in fatal infections and other iatrogenic complications. For example, perineal pads saturated with harsh chemical could not make up for blood lost during a severe hemorrhage or stop an infection acquired during in labor from a break in the aseptic technique. So in spite of all the improvements, teaching hospitals still had a much higher rate of maternal mortality than anyone expected or could explain.
Problem # 5 ~ circa 1910: In 1910, science had not yet come to obstetrics in the United States . At the time, doctoring did not have a particularly good reputation when it came to normal childbirth for healthy women,. The major reason was septicemia or birth-related infections. People couldn’t figure out why they should pay the much high fees of a doctor (instead of a midwife) especially since physician-attended birth was associated with a higher mortality rate for both mothers and babies. From the perspective of the public, the issue was simply that obstetrical care could not dependably address many of the complications that might arise during normal birth and even when it could fix the original problem, the mother might die later on from septicemia. This situation frustrated the obstetrical profession on many levels. It should be noted that about 90% of the miracles of modern medicine had yet to be invented in 1910 – no antibiotics, safe blood transfusion, safe anesthetics and the safer surgical techniques were yet to be developed.
The Fix ~ circa 1910
The obstetrical profession’s attempt to eradicate the infectious diseases of childbirth and simultaneously improve their reputation was predicated on three inter-related ideas. First they redefined the biology of childbirth as basically defective and pathological. In their eyes, the problem was the nature of birth itself and not the quality of obstetrical care provided by doctors. It was the “God made junk” theory — a variation on Freud’s idea that biology was destiny and women got the short end of the stick. Doctors insisted that birth was abnormal because it was associated with damage to the mother’s vaginal tissues. Breaks in the skin of the mother’s birth canal, a fairly frequent occurrence during vaginal birth, permitted deadly bacteria to gain entrance to her blood stream and sometimes cause her and her baby to die.
Second, obstetricians believed that conducting normal birth under conditions of surgical sterility could, for the first time in history, totally eliminate infectious pathogens, and thus make up for the faulty biology of Mother Nature. Childbearing was separated into two halves and care of the laboring women was divided between two professions. Labor was defined as a medical condition to be managed by hospital nurses. Birth was renamed the ‘delivery’, which was now defined as an operative procedure that could only be performed by a physician-surgeon under circumstances of surgical sterility. In order to guarantee the continuing sterility of the operative field, it was necessary to put the mother to sleep with general anesthesia. This was the only dependable way to make sure that laboring women, who were experiencing the normal tumult and physical effort associated with pushing a baby out, would lie quietly on their backs and stay perfectly still during obstetrical manipulations. They also had to be prevented from touching their own genitals or ‘contaminating’ sterile linens and drapes, the doctor’s sterile gloves, sterile instruments, etc by accidentally touching them with their unsterile fingers. Even though anesthetic complications sometimes caused a mother’s death, childbirth under anesthesia was seen as part of the process of protecting women from lethal infections.
Once under the effects of general anesthesia, the mother was in an anti-gravitational position on her back and unconscious. As a result she was no longer able to push effectively, so a generous episiotomy was routinely performed and forceps were used to pull the baby out. Obstetricians saw these interventions as another advantage of birth as a surgical procedure. Episiotomy was thought to spare the mother’s tissues –as well as the delicate tissue of the baby’ brain – from damage sometimes associated with normal birth. Physicians believed that episiotomy, which meant making a nice straight cut in her perineum with scissors, was necessary to preserve the integrity of her pelvic muscles. Episiotomy, in combination with the use of forceps, was assumed to also protect the baby’s head from being battered against the mother’s “iron perineum”.
The third and final part of the obstetrical plan was to eliminate all other forms of maternity care, which they defined as inferior. Non-medical or ‘physiological’ care provided by midwives and country doctors was described as dangerously old-fashioned. Failure to use surgical interventions was believed to cause birth injuries such as cerebral palsy and other problems such as damage to the mother’s pelvic organs. Labor without drugs or birth without anesthesia was decried as intolerably painful and ‘just plain barbaric’. The care of midwives, who were not permitted to use drugs or anesthesia, was claimed to result in an unethical ‘discrimination’ against the poor, who were more likely to use midwives and thus receive “substandard’ care. Universal physician care was assumed to be the only solution to these problems.
Both the public and the medical profession embraced these ideas as a way to permanently end the pain and problems associated with childbirth. This new form of “scientific” obstetrics was seen as one of the first miracles of modern medicine and so society happily concurred with the plan to convert normal childbirth into a surgical procedure. Obstetricians started by getting rid of the midwifery profession. This was coupled with an effort to gradually move all maternity services into hospitals as the final piece of this new and improved standard for 20th century obstetrics. In 1910 organized medicine launched an official campaign to eliminate midwives from the ‘birth business’. By 1920 the number of midwife-attended births dropped from 60% to 13%. The few midwives left were mostly black granny midwives in the segregated South.
This new 20th century form of birth was no longer something to be done by the mother but rather a surgical procedure done by her doctor. Women didn’t give birth to their own babies anymore, instead their doctor delivered the baby. This made physician-attended birth a cross between the notion that babies were brought by the stork and a surgical operation in which unwanted body parts, such as one’s gallbladder or appendix, are ‘taken out’ by the doctor. Of course, women were permitted to be grateful for these life-saving services.
Problem #6 ~ 1941:
Prior to World War II, hospital birth was more a matter of race (white) and class (middle or upper class) than it was a choice predicated on medical needs or the desires of the mother. Doctors did not yet identify women who had high risk pregnancies as needing prophylactic hospitalization. Until 1937 more than 50% of mothers still gave birth at home. These were mostly poor, rural or living in urban tenements and/or black families. However, even a home birth was usually under the medical management of a physician. Doctors who attended labor and birth at home were still a product of the standard obstetrical education and trained to believe that ‘delivery’ was a surgical procedure which usually involved the administration of ether. Then in 1941 American was drawn into the Second World War. A huge percentage of American doctors were drafted into military service and sent overseas as battle surgeons. As a result there were not enough doctors left to meet the need at home. By this time, the profession of midwifery no longer existed, so there was no help from that quarter. What was needed was a way to use the few doctors left behind in a much more efficient way.
The 1940s Fix – The answer in the 1940s was to expand hospital L&D units so that staff nurses, under the supervision of the doctor, could provide care during active labor and help the doctor to precisely time his arrival at the hospital so that he only needed to be physically present during the actual delivery. This system permitted one doctor to attend a dozen or even more births a day, by just stepping from delivery room to delivery room. It was a vast improvement on the old way, which required doctors to drive between the geographically disperse homes of laboring women, a particular problem when gasoline was being rationed.
Assembly line methods of childbirth were refined, permitting laboring women to be admitted in one specially equipped ‘prep’ room, then be moved to a labor ward bed and given ‘twilight sleep’. These drugs were automatically repeated every 3 hours until the baby was born. Large doses of morphine or Demerol mixed with scopolamine caused respiratory depression in the newborn and amnesia in the mother. Under the influence of these drugs the mother was in a semi-comatosed state and unable to get out of bed or to stand, walk or talk. Not much was need in the way of labor support and the hospital certainly was not required to provide the type of one-on-one care that was customary with midwifery care. This made twilight sleep a true ‘labor-saving’ devise from the institution’s standpoint.
Hours or even days later, when the time was right, the mother was moved by stretcher to the delivery room table. The doctor and nurse anesthetist showed up just in time to conduct the surgical procedure of delivery. They put the mother to sleep, cut an episiotomy, extracted the baby with low forceps, manually removed the placenta, sutured the perineal incision. Then nurses moved the unconscious mother by stretcher to the recovery room, while her baby was sent to the nursery to be watched until the mother woke up many hours later. By the end of the Second World War, American hospitals operated quite nicely with a vastly reduced physician presence.
This exact pattern of obstetrical care for hospital labor and delivery was to persist exactly like this for the next 30 years. The only notable changes were the upgrade of anesthetic agents from ether, which is highly toxic, to cyclopropane gas, which is highly explosive. Also the very first, very tentative, very infrequent use of Pitocin to artificially stimulate labor occurred in the early 1960s. Otherwise the L&D nurse or doctor who was a time traveler from the 1920s would be right at home in the 1960s. The only observable difference would be more chrome in the delivery room.
Problem # 7 ~ 1970: There is a subtle expectation in the public mind that miracles of modern medicine, as least as they pertain to obstetrics, will keep on coming ever decade or so. By 1970, things were about 30 years behind the curve. Antibiotics and safer blood transfusions were the last medical miracles to make a big difference in obstetrical care and they’d been around since the end of WWII. The first successful kidney transplant was performed in 1954. In 1967, South African surgeon Christian Barnard performed the first heart transplant. By 1970 our cars were much better, TV was in color, manned space flight to the moon was old hat. However, mothers still got serious hospital-acquired or ‘nosocomial’ infections (and still to get ~ 2005 nosocomial case), babies suffered brain damage and both still died much too often as a direct result of childbirth. In public healthy circles, it was widely recognized that maternal and perinatal deaths in the US were higher than many other developed countries. All this made obstetrics a poor step-sister of modern medicine.
For mothers, the big risk factor was general anesthesia. In 1960, anesthetic-related death was the third leading cause of maternal mortality. The only good news was that fewer mothers died when cyclopropane replaced ether. Eventually there was significant public pressure for more natural forms of hospital childbirth, so that women could at least be awake and aware during labor and husbands and other family members could to be present for the birth.
For babies, the issue was fetal distress during labor and brain damage thought to occur before or during the birth. Obstetricians believed that some form of undetectable fetal distress was the direct cause of cerebral palsy and other permanent neurological damage. If they could just tell when things were going off track and intervene in a timely manner, birth-related death and disability would become a thing of the past. This was the earnest prayer of every obstetrician.
The 1970s Fix ~ Finally obstetrics was getting some well-deserved upgrades in the ‘medical miracles’ department. The two big fixes of the 1970s were electronic fetal monitoring (EFM) and epidural anesthesia. This was the biggest change in obstetrics since 1920s, not quite on a par with heart transplants but still a big deal. The universal use of EFM was seen as a computer-based ‘early warning system’ for fetal distress. When coupled with immediate access to Cesarean section as a rescue operation, EFM was believed to reliably prevent brain damage in the newborn baby and thus permanently eliminate cerebral palsy. It was a prayer answered and an obstetrician’s dream come true.
For mothers the fix was the wide-spread introduction of regional anesthesia. Spinals and epidurals had been around for decades but for some reason, didn’t become popular as obstetric anesthetics until late in the 20th century. Not only did epidural allow the mother be awake and the father present during labor, but when it came time to give birth, the baby was much less likely to have trouble breathing than if she had been given narcotics or different anesthetics. Epidural was much safer that twilight sleep, which could cause such a delay in breathing after the birth that the newborn baby suffered brain damage. The down-side was that mothers had to have IVs running the whole time and frequently required the use of Pitocin to keep the labor moving. Sometimes epidurals caused a precipitous drop in the mother’s blood pressure which resulted in severe fetal distress and required an emergency Cesarean section. Epidurals were also associated with an increased rate of operative deliveries.
Problem # 9 ~ 2000: What seemed, in the 1970s, to be the ‘final’ fix turned out to be like all the obstetrical fixes that preceded it – a problem that started out in life as a solution that was nestled in a problem that was itself, at one time a solution ad infinitum. This long list of medical, surgical, technical or technological fixes all lead to the same place – new problems. EFM was no different. It was not able to prevent cerebral palsy as hoped and expected. EFM is associated with dramatically increased C-section rates without any corresponding improvement in perinatal outcomes. Epidural also is associated with a host of troublesome issues that independently add risk to normal childbirth, including fetal distress and increased operative and C-section rate.
By the year 2000, the routine use of multiple interventions during normal labor was the standard of care. Standard meant that virtually every mother was harpooned to the bed through out active labor by medical equipment and monitoring devices. This often started with artificially breaking the water, hooking the mother up to the continuous EFM and starting an IV. Before long some Pitocin would be added to her IV. This was usually followed by an epidural, which required that an indwelling epidural catheter and administration pump, continuous BP monitor, pulse oximetry, an indwelling bladder catheter, a urine bag hooked to the side of the bed all be added to the mix of medical equipment. Finally an oxygen mask was put on the mother’s face when the EFM seems to convey worrisome information to the nurse.
Like the scene in the Monty Python movie “The Meaning of Life”, one can hardly find the patient in the tangle of equipment, wires, tubes, and electronic leads and yes, the machine that constantly goes “peep”. Studies of healthy women giving birth in the year 2002 found that an average of seven or more medical and surgical interventions are routinely used for every healthy mother cared for under hospital-based obstetrical management.
Now here is the really bad news: The net effect is that anti-gravitational positions are virtually mandated by the holy trinity of modern childbirth – continuous EFM, the epidural and the supporting cast of medical paraphernalia and protocols. As a result women have to push their babies straight uphill and around a 60-degree curve while lying on their back. All this uphill pushing is hard for the mother, especially as she is anesthetized and often can’t feel her body or figure out exactly how to work with it. It’s also hard on her body and it’s hard on the baby. In fact, sometimes it’s impossible. When that happens, the additional intervention of episiotomy is often tried, then attempts to deliver with vacuum extractor; when that doesn’t work forceps are tried and when all else fails, a Cesarean section is done. In far too many cases, this results in maternal incontinence and other pelvic floor problems after the birth or later in her life. Many people have begun to question this scenario and to wonder if it wouldn’t be better to just do the C-section right at the get-go and skip all the anxiety, pain and sequential use of invasive technology.
The Fix for 2000 ~ To the obstetrical profession the answer is obviously “Yes”. A high percentage of obstetricians are convinced that elective or maternal choice Cesarean is the ‘final fix’ and should replace vaginal birth as the standard of care. In the year 2000, the obstetrical profession started aggressively promoting the idea of the ‘elective’ or medically unnecessary use of Cesarean as the Rolls Royce of childbirth. The American College of Obstetricians and Gynecologists (ACOG) has fully-approved the performing of medically unnecessary Cesarean as an ‘ethical’ activity for its physicians. At this moment, America stands at the cusp of what many in the obstetrical profession hope will lead to the ‘patient-choice’ Cesarean becoming the “standard of care” for all childbirth in the US by 2010.
Problem # 10 ~ 2006: For the last hundred years, maternity care in the US has been organized around a system of hospital interventions that are a left-over from the 19th century. This pseudo-science has perpetuated an ever-expanding appetite for labor stimulating drugs, electronic fetal monitoring, anesthesia, episiotomy, forceps, manual exploration of the uterus after delivery and most of all, the liberal use of Cesareans.
This brings us back around in a perfect circle to 1910, when American obstetricians first decreed that the problem with birth was the nature of birth itself and not the quality of care provided by doctors. We are to believe that women – at least modern women — are just not made for having babies vaginally. In 1910, normal birth was renamed the ‘delivery’ by the obstetrical profession and defined as an operative procedure. Now the perceived solution is just one more little step along that path to surgical nirvana, the next logical step – no longer just vaginal birth as a surgical procedure but birth totally replaced by a surgeon and surgery – a planned and scheduled Cesarean-section. Obstetrics may have achieved its idea of perfection but as a national policy for maternity care, this is a perfect nightmare.
Operative deliveries are associated with post-operative complications that include hemorrhage, emergency hysterectomy, pulmonary embolism and infection. Medicalized labor and operative delivery are also associated with delayed complications such as stress incontinence and pelvic organ prolapse. Cesarean section is associated with 33 specific route-of-delivery complication, including a doubling of maternal deaths, compared to only 4 for spontaneous vaginal birth. Cesareans can result in secondary infertility and downstream complications in future pregnancies which include stillbirth, uterine rupture and emergency hysterectomy. Post-cesarean mothers have a higher rate of long-term psychological issues such as PTSD and postpartum depression. Babies born by cesarean section have lower rates of breastfeeding and increased rates of asthma in childhood and as adults.
Of course, Cesareans are the gift that keeps on giving as once done, all future pregnancies are destined to be delivered by repeat surgeries. This could be considered an obstetrical form of Munchausen’s Disease as medical over-treatment results in complications from which obstetricians then get to rescue their patients. This cost of all this is from three to ten times as much as normal birth and means that the US is hemorrhaging scarce healthcare dollars on healthy women with normal pregnancies.
A Maybe–Maybe-not Fix, circa 2006: The conduct normal childbirth in hospitals under conditions of surgical sterility was originally done because it was the only method available in the late 1800s to prevent the epidemic of puerperal sepsis in institutional settings. Even though it was obvious that aggregating pregnant women in an institutional setting was a basic part of the problem, the medical profession concluded that hospitalization for birth was necessary in order to make clinical training available to medical students. It is a fluke of history that we got caught in the cross hairs of that singular event, which so influenced and defined the development of maternity care for healthy women in the US and left us with a system that has systematically refused to teach, learn or utilize physiological management for nearly a hundred years.
Organized medicine has spared no expense in their efforts to convince the public, the press, the legislatures and the courts that overwhelming medicalization is good for mothers and is worth any price, as it is buying us better babies. Perceived problems simply mean we need to throw more money at even more expensive forms of obstetrics. We have never yet had had a science-based system of maternity care in the United States or even a national maternity care policy that sees a scientific system as a desirable or attainable goal. Unfortunately, the story of iatrogenesis is not yet over.
Now there is no hope to end this madness except for you and me. Unless we elevate the public discourse, unless we challenge the illogical idea that ‘doctors know best’, unless we demand that maternity care for healthy women be science-based as are other forms of health care, we will indeed all live to see the death of normal birth.
