
A super-high-tech OR with a specialized staff of 18 — doctors, nurses and others — to perform a Cesarean hysterectomy for “placenta percreta”. This a well-known and frequent post-op complication of previous Cesareans surgeries in which the placenta invades the muscular wall of the uterus and grows deeply into other pelvic organs such as the mother’s bladder in a subsequent pregnancy. The rate of massive uncontrollable maternal hemorrhage is so great that even with the very best care in the best-equipped hospitals with 5 different surgeons, other medical specialists and special radiology equipment in the OR, the maternal death rate is from 7 to 10 percent.
The Obstetrical Standard of Care in the US – Historically irrational, fundamentally flawed
As currently configured in the US, the medicalized model makes it virtually impossible for obstetrically-trained birth attendants to use physiologically-based methods. Physiological management is not the ‘customary’ practice of those trained in the surgical specialty of obstetrics and it is not taught to interns or obstetrical residents.
Ironically, the entire tradition of physiological care has been defined by the medical profession as a substandard or negligent form of care for the nearly a hundred years. This puts obstetricians in a straightjacket and childbearing women in jeopardy.
Many complicated historical and economic issues contribute to an institutionalized inability to provide physiologic care but at its most basic level, the problem is perpetuated by the way the standard of care for obstetrics is defined.
Legally the ‘quality’ of care that any individual obstetrician is held to is not primarily determined or defined by what is physiologically indicated or what can be proven via evidence-based science to be the safer or better choice.
Instead, the standard for obstetrical care, which is legally a surgical specialty, is determined by the customary practices of other obstetricians, irrespective of whether or not such customs are good or bad, safe or risky, evidence-based or merely reflect the personal ‘preferences’ of local obstetricians. It’s crazy enough to make any sane person cry.
Examples of this are too numerous to list, but they routinely include:
- routine use of multiple ultrasounds during prenatal care
- induction of labor at 39-40 weeks
- being ‘bedded’ during labor
- ordering IVs and continuous EFM on admission to the hospital,
- using IV Pitocin to accelerate labor at a certain predetermined rate of cervical dilatation
- scheduling elective Cesareans whenever ultrasound estimates of the baby’s weight are over 4000 grams
- scheduled repeat C-section simply based on the mother’s a previous Cesarean but without any medical or prenatal complication requiring surgical delivery
Obstetricians who don’t follow the crowd are penalized. They risk losing referrals from other physicians and don’t get offered a seat on the department’s many committees. If they still don’t get the hint, they may lose their hospital admitting privileges or their malpractice coverage.
After the fact, the aggregate of individual physician preferences simply becomes, without any further oversight or accountability, the de facto standard of care – good, bad or indifferent, if other obstetricians are doing it, you have to do it, and if others don’t do something (like physiologically-based management of normal labor, you get a dispensation as well.

Standard version of normal vaginal birth conducted as the surgical procedure of “normal vaginal delivery”
Once something becomes official policy, the influence and effect it has on every obstetrician in that community is similar to the federal government’s stated foreign policies on members of the US military. Every good soldier is expected to follow the proscribed guidelines to the letter and is subject to disciplinary actions if s/he should fail to do so. Not even the generals have the individual right to change or suspend the official rules as determined by the Powers That Be.

Preparing the mother-to-be for Cesarean delivery, OR staff getting ready, anesthesiologist giving the patient oxygen and a betadine antiseptic has been painted over her pregnant belly and legs to sterilize the mother’s skin.
This form of external control also applies to obstetricians thru the position statements of the American College of Obstetricians and Gynecologists, ACOG technical bulletins and formal policies, in combination with customary practices as defined by experts from within the obstetrical profession and the ‘community standard’ – local custom.
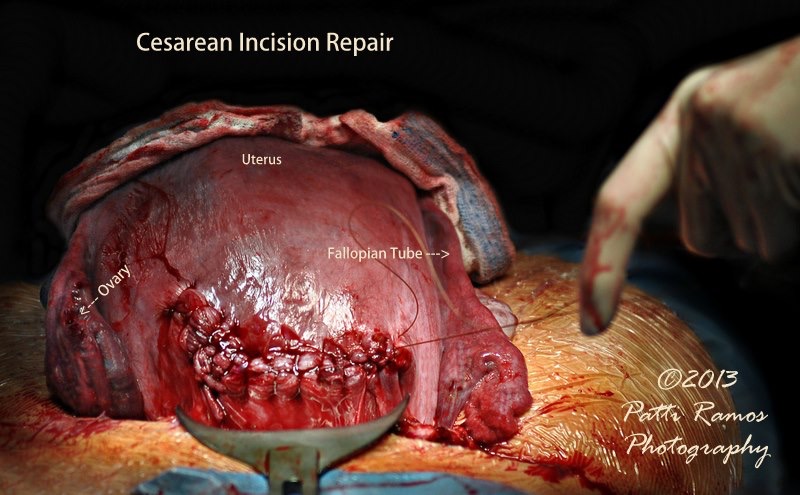
Externalization of the uterus during Cesareans surgery (after the baby has been delivered). The incised uterus is pulled up and out of the mother’s abdomen and then laid on top of her abdomen so it is easier for the surgeon to see while he or she is suturing the incision that the baby was removed through. This view is looking up from the mother’s legs, with the ‘bladder retractor’ visible at the bottom of the picture (the wide metal instrument just below the uterine suture line). Surgeon’s gloved hand is to the right.
The lay public views the obstetrical profession from a great distance and mistakenly thinks things look pretty wonderful. Seen from the moon, many envy physicians for what seems to be an absolute degree of autonomy and power greater than any other group of individuals they know.
Like military generals like their war toys and relish opportunites to do what they were trained for, obstetrician-gynecologists, as trained surgeons, naturally like to do what they were trained for, which is of course surgery.
But sadly, the close and personal view of obstetrics as a surgical specialty reveals an astonishing (and unexpected) lack of both autonomy and control for doctors. For many obstetricians, the pressure to conform is an extreme incongruity with what they thought it meant to ‘deliver babies’. They are bitterly disappointed by the lack of personal control they experience in their professional life, and unable to reconcile their daily reality with what they thought the practice of medicine would be like. Many of these doctors leave the medical profession after a decade or so.
All of this combines to make childbearing in the 21st century something of a trick with mirrors – it looks like it is the most advanced its ever been and like doctors and nurses and labor patients (and expectant fathers) are happier than they have ever been – a nirvana in pink and blue.
But just slightly below the surface, its very different. The labor and delivery suites of contemporary hospitals seem dramatically improved over the restrictive architecture and policies of earlier decades, but it is equally and sometimes even more difficult for childbearing women to have a physiologically-managed labor and spontaneous birth today than even five years ago.
In particular, women with obstetrically unpopular situations – VBAC, breech, twins, big baby, a small-for-dates baby, prolonged rupture of membranes, women with other rare or unusual circumstances that are risk factors but not themselves complications — still find that only way to avoid unwanted interference is to labor unattended at home until the very last minute. Then they leave for the hospital and hope to give birth before the obstetrical machine can get geared up to intervene in ways they don’t want or to ‘deliver’ them via Cesarean section.
If the US is to successfully compete in the global economy of the 21st century, we must reconsider the illogical idea of standards as the collective preferences of the obstetrical profession. This irrational system prevents the US from developing a cost-effective maternity care system that utilizes physiological care for healthy women.
Most of the world is already using cost-effective methods of maternity care — being left behind is not an option.

