Easy-2-share Link: https://tinyurl.com/y8tjlqh5
When and How to Push:
Providing the Most Current Information About Second-Stage Labor to Women During Childbirth Education
Abstract
 Childbirth educators can have a significant impact on safe care for mothers and babies during the second stage of labor. In this guest editorial, educators are encouraged to make sure they are knowledgeable about the latest evidence for best second-stage-care practices so they can adequately prepare women to advocate for themselves during this time.
Childbirth educators can have a significant impact on safe care for mothers and babies during the second stage of labor. In this guest editorial, educators are encouraged to make sure they are knowledgeable about the latest evidence for best second-stage-care practices so they can adequately prepare women to advocate for themselves during this time.
Keywords: second-stage labor, childbirth education
 Childbirth educators can have a significant impact on safe care for mothers and babies during labor and birth. Pregnant women and their families need accurate, science-based information to advocate for themselves and their care in full partnership with nurses, nurse midwives, and physicians.
Childbirth educators can have a significant impact on safe care for mothers and babies during labor and birth. Pregnant women and their families need accurate, science-based information to advocate for themselves and their care in full partnership with nurses, nurse midwives, and physicians.
In addition to focusing on what to expect during labor and how to handle contraction pain and discomfort, pregnant women are often concerned about their ability to push their baby out when the time comes. They may hear from friends and family of long, exhausting hours of pushing while, in contrast, they observe television portrayals of women who usually give birth after only one or two pushes. Information presented in childbirth preparation classes provides a foundation for expectations of how care will be provided and what women need to know to safely complete the last part of labor before birth.
THE “OLD WAY”
 The “old way” of assisting women during second-stage labor typically involves pushing immediately at 10 cm regardless of whether the woman has an urge to push; telling the woman to take a deep breath and hold it (closed-glottis pushing) while someone (partner, nurse, nurse midwife, or physician) counts to 10 during at least four to five pushing efforts per contraction as the woman lies in the supine lithotomy position (often using stirrups); and a care provider forcing the woman’s legs back against her abdomen (Simpson & James, 2005). These techniques have the potential to cause harm to the mother and baby (Simpson, 2004).
The “old way” of assisting women during second-stage labor typically involves pushing immediately at 10 cm regardless of whether the woman has an urge to push; telling the woman to take a deep breath and hold it (closed-glottis pushing) while someone (partner, nurse, nurse midwife, or physician) counts to 10 during at least four to five pushing efforts per contraction as the woman lies in the supine lithotomy position (often using stirrups); and a care provider forcing the woman’s legs back against her abdomen (Simpson & James, 2005). These techniques have the potential to cause harm to the mother and baby (Simpson, 2004).
A full discussion of the potential harm in the traditional approach and recommendations for practice changes are presented in the Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN) Evidence-Based Clinical Practice Guideline: Nursing Management of the Second Stage of Labor (2000).
A recent review of the literature (Roberts, 2002) provides additional information. Staying current with rigorous evidence related to labor and birth is crucial for childbirth educators so they are able to provide women and their families with the best information available to promote safe care.
A BETTER WAY BASED ON CURRENT EVIDENCE
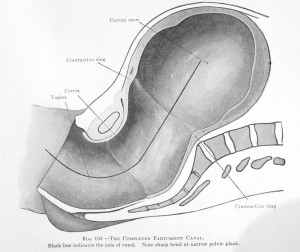
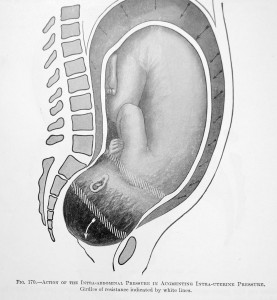
The “J” shape of a woman’s pelvis means the baby must change directions as it spins around the bottom curve of the letter “J” while going under the pubic bone and simultaneously moving up and out as it’s being born. If the mother is lying on her back, the curve of the “J” requires her to push the baby uphill, towards the ceiling, which means working against the forces of gravity (i.e. anti-gravitational position)
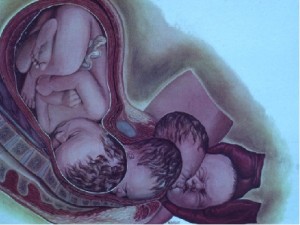
A better approach based on current evidence is to delay pushing until the woman feels the urge to push. With epidural anesthesia, pushing can be delayed up to 2 hours for nulliparous women and up to 1 hour for multiparous women (Hansen, Clark, & Foster, 2002; Simpson & James, 2005).
Shows the baby tracking with the letter “J” (the technical term for bend at the bottom is the “Curve of Carus”; its head turns sideways to slip under the mother’s pubic bone (head #1); then turns face down as the crown of its head begins to distend the mother’s perineum (head #2); the head moves uphill as it literally crowns and the baby is born (head #3) and then the head turns to face sideways in order to lines up with the rest of the baby’s body (head #4).
There are two phases to the second stage of labor: the initial latent phase and the active pushing phase (Roberts, 2002). The most stressful period of labor for the fetus is the active pushing phase; thus, shortening this phase minimizes fetal stress and promotes fetal well-being (Caldeyro-Barcia, 1979; Caldeyro-Barcia et al., 1981; Roberts, 2002; Simpson & James, 2005).
When pushing is delayed until the woman’s urge to push, there are fewer fetal heart rate (FHR) decelerations and less of a negative effect on fetal acid-base status and oxygenation (Caldeyro-Barcia et al., 1981; Hansen et al., 2002; Nordstrom, Achanna, Nuka, & Arulkumaran, 2001; Piquard, Schaefer, Hsiung, Dellenbach, & Haberey, 1989; Roemer, Harms, Buess, & Horvath, 1976; Simpson & James, 2005; Thomson, 1993).
 The latent phase is an ideal time to allow the woman to rest in preparation for pushing efforts at the appropriate time (Roberts, 2002). When the time is right for pushing, the best approach based on current evidence is to encourage the woman to do whatever comes naturally; for example, bearing down and holding it as long as she can, rather than insisting that she hold her breath for 10 to 15 seconds to the count of 10 (AWHONN & InJoy Videos, 2006).
The latent phase is an ideal time to allow the woman to rest in preparation for pushing efforts at the appropriate time (Roberts, 2002). When the time is right for pushing, the best approach based on current evidence is to encourage the woman to do whatever comes naturally; for example, bearing down and holding it as long as she can, rather than insisting that she hold her breath for 10 to 15 seconds to the count of 10 (AWHONN & InJoy Videos, 2006).
{Editor’s note: As an L&D nurse during the “knock’em out, drag’em out” Twilight Sleep era (Dark Ages deep South 1960s), heavily medicated women can’t and don’t pay any attention to what you tell them. They pushed when their body gave them the physiologic stimulus and that pushing rarely ever lasted longer than 6 seconds, but they usually had 3 “urges” for each UC with a nice deep breath between each push}.
Prolonged maternal breath-holding results in maternal apnea and negative maternal hemodynamic changes that lead to decreased blood flow to the placenta and, ultimately, negative consequences for the fetus (Barnett & Humenick, 1982; Caldeyro-Barcia et al., 1981; Simpson & James, 2005). Three to four pushing efforts of 6 to 8 seconds in length per contraction are physiologically appropriate (AWHONN, 2000; Roberts, 2002; Simpson & James, 2005).
“When the time is right for pushing, the best approach based on current evidence is to encourage the woman to do whatever comes naturally.”
Positioning is an important component of safe and effective pushing. An upright position or lateral position works better than supine positioning and has fewer negative maternal hemodynamic changes (Roberts, Algert, Cameron, & Torvaldsen, 2005). Encourage the woman to choose a position of comfort and to change positions as often as needed.
 Forcing women’s legs back against their abdomen during pushing should be avoided because this results in stretching the perineum and increases the risk of perineal lacerations (Sampselle & Hines, 1999; Simpson & James, 2005).
Forcing women’s legs back against their abdomen during pushing should be avoided because this results in stretching the perineum and increases the risk of perineal lacerations (Sampselle & Hines, 1999; Simpson & James, 2005).
No evidence suggests that manual massaging or stretching the perineum is beneficial, and many women find this technique uncomfortable (Albers, Sedler, Bedrick, Teaf, & Peralta, 2005).
Positioning is an important component of safe and effective pushing.
PROMOTING FETAL WELL-BEING
 It is particularly important to recognize non-reassuring FHR patterns during the second stage of labor and to intervene appropriately (AWHONN & InJoy Videos, 2006). A commonly held myth suggests that it is better to “get the baby out” rather than to allow the mother to rest and the fetus to recover.
It is particularly important to recognize non-reassuring FHR patterns during the second stage of labor and to intervene appropriately (AWHONN & InJoy Videos, 2006). A commonly held myth suggests that it is better to “get the baby out” rather than to allow the mother to rest and the fetus to recover.
Many care providers fail to realize that their aggressive coaching techniques are the cause of non-reassuring FHR patterns (Simpson, 2004). If the fetus does not respond well to pushing, the best approach is to stop pushing temporarily and let the fetus recover (Freeman, Garite, & Nageotte, 2003).
 If the fetus continues to respond poorly—as evidenced by abnormal changes in the FHR and recurrent variable or late decelerations—and there is a compelling reason to continue pushing, pushing with alternate contractions works best. It may be necessary to have the woman push with every other contraction or every third contraction to maintain a reassuring FHR pattern (AWHONN & Injoy Videos, 2006; Freeman et al., 2003).
If the fetus continues to respond poorly—as evidenced by abnormal changes in the FHR and recurrent variable or late decelerations—and there is a compelling reason to continue pushing, pushing with alternate contractions works best. It may be necessary to have the woman push with every other contraction or every third contraction to maintain a reassuring FHR pattern (AWHONN & Injoy Videos, 2006; Freeman et al., 2003).
The woman should be assisted to a lateral position. A baseline FHR should be able to be identified between contractions.
If the fetus does not respond well to pushing, the best approach is to stop pushing temporarily and let the fetus recover.
If the fetus does not tolerate pushing and the woman has received an epidural, the passive fetal descent approach is quite useful (AWHONN, 2000; AWHONN & InJoy Videos, 2006). Evidence suggests that, for women with epidurals, coached pushing beginning immediately at 10 cm does not result in a clinically significant decrease in the length of the second stage (Fraser et al., 2000; Hansen et al., 2002; Mayberry, Hammer, Kelly, True-Driver, & De, 1999; Roberts, 2002).
 Passive fetal descent will result in about the same length of the second stage for women with epidural anesthesia as does the coached-pushing approach. Patience and encouragement are most helpful, rather than insisting that the woman push before it is appropriate and/or when the FHR is nonreassuring.
Passive fetal descent will result in about the same length of the second stage for women with epidural anesthesia as does the coached-pushing approach. Patience and encouragement are most helpful, rather than insisting that the woman push before it is appropriate and/or when the FHR is nonreassuring.
The FHR pattern should be used as an indicator as to how well the fetus responds to second-stage labor (Simpson, 2004). Recurrent variable or late decelerations during the second stage are associated with respiratory acidosis at birth (Parer, King, Flanders, Fox, & Kilpatrick, 2006). I
n addition, the fetus may develop metabolic acidosis if this type of pattern continues over a long period (Parer et al., 2006). These babies are difficult to resuscitate and may not transition well to extrauterine life.
THE ROLE OF CHILDBIRTH EDUCATORS AS MEMBERS OF THE PERINATAL TEAM

Ideally, clinical practice is consistent with the latest evidence; however, in some labor units, care providers may not be completely up-to-date on best second-stage labor care. Pregnant women and their families can overcome this limitation if they are fully informed and prepared to ask for selected care processes.
Childbirth educators help to facilitate this knowledge. For women who choose to use a birth plan, consider sharing the information in Table 1 to add to their birth plan as requests for second-stage labor care.
TABLE 1
Birth Plan Content for Second-Stage Labor
| • Please wait until I feel the urge to push before asking me to push. |
| • Please allow me to do whatever comes naturally when pushing (I may or may not choose to hold my breath). |
| • Please do not count to 10 during each of my pushing efforts. Allow me to bear down and hold it as long as I feel comfortable. |
| • Please let me know how I am doing and offer words of encouragement. |
| • Please allow me to position myself for comfort and help me to change position often. |
| • Please do not push my legs back while I am pushing. Allow me to keep my feet flat on the bed if I choose to push in that position. |
| • Please watch how my baby tolerates pushing and use the fetal heart rate pattern to guide your pushing directions. |
| • Please do not massage or stretch my perineum while I am pushing. Allow my perineum to stretch naturally. |
Often, childbirth educators are not well connected to other members of the perinatal team; however, they can take the initiative to be more active team members by sharing information and participating in discussions about the latest evidence applicable to clinical practice during labor and birth.
Make an effort to coordinate childbirth education content with those who provide the care during labor and birth. Arrange to observe clinical practice during second-stage labor.
If practices are not consistent with current evidence and AWHONN clinical guidelines, work with care providers to promote change. Discuss best practice during second-stage labor with physicians and nurse leaders. Offer to share the information in Table 2. Use the AWHONN (2000)Evidence-Based Clinical Practice Guideline and AWHONN and InJoy Videos (2006) Second Stage Labor Support production as a basis for this discussion. Include additional pertinent literature as well, some of which is listed in the reference list below.
Table 2
Physiologic-Based, Second-Stage Labor Practices
| • For women with epidural anesthesia who do not feel the urge to push when they are completely dilated, delay pushing until the urge to push is felt (up to 2 hours for nulliparous women and up to 1 hour for multiparous women). |
| • Use upright positioning with the woman’s feet flat on the bed. Change to a lateral position or other positions of comfort as necessary. |
| • Avoid forcing the woman’s legs back against her abdomen. |
| • Discourage prolonged breath-holding. Instead, instruct the woman to bear down and allow her to choose whether or not to hold her breath while pushing. |
| • Discourage more than three to four pushing efforts with each contraction and more than 6 to 8 seconds of each pushing effort (avoid counting to 10 with each pushing effort). |
| • Take steps to maintain a reassuring fetal heart rate (FHR) pattern while pushing. Push with every other or every third contraction if necessary to avoid recurrent FHR decelerations. Reposition as necessary to treat FHR decelerations. Use the fetal response to pushing as a guide for second-stage care. |
| • Avoid uterine hype-rstimulation during the second stage of labor. Make sure that contractions are no closer than every 2 to 3 minutes while pushing. Titrate oxytocin accordingly, use an intravenous fluid bolus of lactated Ringer’s solution, and reposition to decrease contraction frequency. |
| • Allow the woman’s perineum to stretch naturally rather than using manual massage or stretching. |
 Childbirth educators can influence unit practice to make second-stage labor care as safe as possible. Do whatever it takes to become a visible, highly knowledgeable member of the perinatal team. We are all invested in the most optimal birth outcomes for mothers and babies. Working together is our best hope for success.
Childbirth educators can influence unit practice to make second-stage labor care as safe as possible. Do whatever it takes to become a visible, highly knowledgeable member of the perinatal team. We are all invested in the most optimal birth outcomes for mothers and babies. Working together is our best hope for success.
Childbirth educators can take the initiative to be more active team members by sharing information and participating in discussions about the latest evidence applicable to clinical practice during labor and birth.
References
- Albers L. L, Sedler K. D, Bedrick E. J, Teaf D, Peralta P. Midwifery care measures in the second stage of labor and reduction of genital tract trauma at birth: A randomized trial. Journal of Midwifery and Women’s Health. 2005;50(5):365–372. [PMC free article] [PubMed] [Google Scholar]
- Association of Women’s Health, Obstetric and Neonatal Nurses [AWHONN]. Evidence-based clinical practice guideline: Nursing management of the second stage of labor. 2000 Washington, DC: Author. [Google Scholar]
- Association of Women’s Health, Obstetric and Neonatal Nurses [AWHONN] & InJoy Videos (Producers). High-touch nursing care during labor. Volume 3: Second stage labor support. 2006 . (Available from InJoy Birth & Parenting Videos, 7107 La Vista Place, Longmont, CO 80503) [Google Scholar]
- Barnett M. M, Humenick S. S. Infant outcome in relation to second stage labor pushing method. Birth and the Family Journal. 1982;9:221–229. [Google Scholar]
- Caldeyro-Barcia R. The influence of maternal bearing-down efforts during second stage on fetal wellbeing. Birth and the Family Journal. 1979;6:17–21. [Google Scholar]
- Caldeyro-Barcia R, Giussi G, Storch E, Poseiro J. J, Kettenhuber K, Ballejo G. The bearing down efforts and their effects on fetal heart rate, oxygenation, and acid-base balance. Journal of Perinatal Medicine. 1981;9(Suppl. 1):63–67. [PubMed] [Google Scholar]
- Fraser W. D, Marcoux S, Krauss I, Douglas J, Goulet C, Boulvain M. Multicenter randomized controlled trial of delayed pushing for nulliparous women in the second stage of labor with continuous epidural analgesia. American Journal of Obstetrics and Gynecology, 182. 2000;(5):1165–1172. for the PEOPLE (Pushing Early or Pushing Late with Epidurals) Study Group. [PubMed] [Google Scholar]
- Freeman R. K, Garite T. J, Nageotte M. P. 2003. Fetal heart rate monitoring (3rd ed.). Philadelphia: Lippincott Williams & Wilkins. [Google Scholar]
- Hansen S. L, Clark S. L, Foster J. C. Active pushing versus passive fetal descent in the second stage of labor: A randomized controlled trial. Obstetrics and Gynecology. 2002;99(1):29–34. [PubMed] [Google Scholar]
- Mayberry L. J, Hammer R, Kelly C, True-Driver B, De A. Use of delayed pushing with epidural anesthesia: Findings from a randomized controlled trial. Journal of Perinatology. 1999;19(1):26–30. [PubMed] [Google Scholar]
- Nordstrom L, Achanna S, Nuka K, Arulkumaran S. Fetal and maternal lactate increase during active second stage of labour. British Journal of Obstetrics and Gynaecology. 2001;108(3):263–268. [PubMed] [Google Scholar]
- Parer J. T, King T, Flanders S, Fox M, Kilpatrick Fetal acidemia and electronic fetal heart rate patterns: Is there evidence of an association? Journal of Maternal-Fetal and Neonatal Medicine. 2006;19(5):289–294. [PubMed] [Google Scholar]
- Piquard F, Schaefer A, Hsiung R, Dellenbach P, Haberey P. Are there two biological parts in the second stage of labor? Acta Obstetricia et Gynecologica Scandinavica. 1989;68(8):713–718. [PubMed] [Google Scholar]
- Roberts C. L, Algert C. S, Cameron C. A, Torvaldsen S. A meta-analysis of upright positions in the second stage of labor to reduce instrumental deliveries in women with epidural anesthesia. Acta Obstetricia et Gynecologica Scandinavica. 2005;84(8):794–798. [PubMed] [Google Scholar]
- Roberts J. E. The “push” for evidence: Management of the second stage. Journal of Midwifery and Women’s Health. 2002;47(1):2–15. [PubMed] [Google Scholar]
- Roemer V. M, Harms K, Buess H, Horvath T. J. Response of fetal acid-base balance to duration of the second stage of labour. International Journal of Gynaecology and Obstetrics. 1976;14(5):455–471. [PubMed] [Google Scholar]
- Sampselle C, Hines S. Spontaneous pushing during birth—Relationship to perineal outcomes. Journal of Nurse Midwifery. 1999;44(1):36–39. [PubMed] [Google Scholar]
- Simpson K. R. Second stage labor care. MCN: The American Journal of Maternal Child Nursing. 2004;29(6):416. [PubMed] [Google Scholar]
- Simpson K. R, James D. C. Effects of immediate versus delayed pushing during second-stage labor on fetal well-being. Nursing Research. 2005;54(3):149–157. [PubMed] [Google Scholar]
- Thomson A. M. Pushing techniques in the second stage of labour. Journal of Advanced Nursing. 1993;18(2):171–177. [PubMed] [Google Scholar]
Articles from The Journal of Perinatal Education are provided here courtesy of Lamaze International
