Originally published March 2019 ~ New Intro & Overview
Easy shortcut to share –> http://tinyurl.com/y4ezxjsz ~ word count 2,866 ~
Identifying the false association (and failed strategy) surrounding the routine use of continuous electronic fetal monitoring (EFM) as the universal standard and the associated increase in Cesarean surgery performed for a ‘non-reassuring’ EFM tracing.
The purpose of this medical and legal strategy was to:
-
Prevent cerebral palsy and other permanent neurological damage in newborn babies
-
Protect hospitals and obstetrical professionals from childbirth-related malpractice suits
 Intro & Overview
Intro & Overview
This is a series of posts on the safety, expense, social consequences and ethical considerations of the current policies and protocols for electronic fetal monitoring in the US as the obstetrical standard of care.
The ‘what’ and ‘why’ of fetal monitoring
Listening regularly to the rate and rhythm of the unborn baby’s heart during the labor and birth is a standard protocol used routinely during the active labor and birth of babies born in developed countries. It’s clearly appropriate to monitor the unborn baby during the biological stress of labor.
The question is not if we should monitor the unborn baby during labor, but how — regularly scheduled listening with fetoscopes and Dopplers, or continuous electronic monitoring? What is the scientific evidence and does it provide the information we need to make the best decision for each laboring woman?
Fetal Monitoring Protocols, beginning with the verbs of Auscultation
 From the invention of a special type of stethoscope known as ‘fetoscope’ in the late 1800s until 1973, the universal standard of care during labor required professional birth attendants to regularly listen, count and record the fetal heart rate, and if it was not within the normal range, to take appropriate action.
From the invention of a special type of stethoscope known as ‘fetoscope’ in the late 1800s until 1973, the universal standard of care during labor required professional birth attendants to regularly listen, count and record the fetal heart rate, and if it was not within the normal range, to take appropriate action.
Monitoring the fetal heart rate with a fetoscope or doppler is called auscultation. This unfamiliar word, which is pronounced aw – skull – tah – tion— describes the simple act of listening to biological sounds in the bodies of human and animals, usually from hollow organs such as heart, lung, or bowel, and using a device such as a stethoscope, fetoscope or hand-held electronic doppler.
When listening to the fetal heart, auscultation also requires the use of a wristwatch or a wall clock with a second hand so the number of heartbeats per minute can be counted, as well as the presence or absence of other heart-related characteristics, such as regularity, variability, accelerations (transient speeding up of the FHR) and decelerations (a temporary slowing of the FHR).
Fetal heart sounds can also be heard by placing your ear directly against the mother’s pregnant abdomen, or rolling up a piece of paper and making it into a tube and then using that to listen. These simple ideas led to the invention of the stethoscope in 1816 by a Parisian physician (René Laennec) because it was embarrassing to place his ear directly on a woman’s unclothed chest in order to listen to her heart.
For healthy women with normal term pregnancies, the protocol for auscultation during active labor requires labor and birth attendants to listen with a fetoscope or hand-held Doppler for at least one full minute (longer if indicated) and from time to time, listening during a contraction and for 15 seconds after it has ended.
In addition to counting the baby’s heart rate per minute (beats-per-minute or bpm), birth attendants also note its rhythm (regular or irregular), listen for normal variability (slight transient increase in rate over several seconds and a return to baseline) and a significant or prolonged increase in the baseline rate (accelerations) or decrease (decels). When decels are heard, the frequency and pattern of repeating decelerations is also noted.
Auscultation protocols based on the Various Stages and Phases of Labor
Latent Labor: During the very early or latent (‘warm-up’) phase of first stage labor, regularly scheduled monitoring (hourly or more often) of healthy unborn babies is not necessary, since early contractions are brief in length, mild in strength, and not very frequent. This warm-up phase of labor, which typically lasts from 4 to 48 hours, generally isn’t stressful in a low-risk pregnancy with a healthy term fetus. Also this period occurs before the mother-to-be is admitted to the hospital or birth center.
When the parents are planning a home birth, this early phase occurs before their birth attendants are physically present and have begun to provide standard intrapartum care, which is not until the mother is in an active labor pattern and has a cervical dilatation of 5-6 centimeter if a first baby, or 3-4 cms for mothers who have given birth one or more times before.
But if the mother-to-be in latent labor is admitted to a hospital L&D unit or birth center, or laboring at home and her birth attendant has begun monitoring the labor, the unborn baby’s heart rate will be listened to every hour as long as the mother is awake. In OOH settings, the mother-to-be is generally not awaken to listen to the baby.
Active First Stage Labor: After things have progressed to active first stage labor (contractions 5 minutes or less, lasting 60 seconds or longer and consistent for more than an hour) the FHR is to listened to every 30 minutes, or more frequently if indicated.@@@
The protocol for auscultation also requires a labor room nurse, midwife or physician to be consistently present in the room during the active phases of the woman’s labor. In addition to listening and keeping track of significant changes in the fetal heart tones, auscultation includes direct observation of the mother’s physical and mental well-being and the nature and progress of her labor as it affects her and her fetus.

Second or Pushing Stage of Labor: After full dilation, the pushing stage begins. Generally this includes two distinct phases, with the frequency depending of fetal monitoring being based on the phase. As the mother pushes the baby’s down into the birth canal (the descent phase), birth attendants listen every 15 minutes or so.
During the perineal phase, when the baby is being pushed out of the birth canal and its head is subjected to more direct pressure, the fetal heart is listened to after every second or third other contraction or approximately every 5 minutes (more frequently if indicated).
Charting: Each time information is collected on the unborn baby’s heart rate and rhythm it is recorded on the mother’s chart. This data is carefully tracked and used to confirm the continuing well-being of the unborn baby or alert the birth attendants of a potentially problem. If a serious abnormality is in the fetal heart rate or its pattern is detected, the situation is evaluated and when needed, medical or surgical interventions are used.
 Usually, the mother-to-be requires and greatly benefits from the support and assistance provided by labor and birth attendants. On-going one-on-one care helps her cope more effectively with the normal anxiety, pain, and physical stress of her labor, which helps reduce the need for medical and surgical interventions.
Usually, the mother-to-be requires and greatly benefits from the support and assistance provided by labor and birth attendants. On-going one-on-one care helps her cope more effectively with the normal anxiety, pain, and physical stress of her labor, which helps reduce the need for medical and surgical interventions.
Studies over the last half-century that compared auscultation to electronic fetal monitoring show no difference in outcome (neither better or worse) for the newborn babies of healthy women with normal pregnancies.
The nouns of Electronic Fetal Monitoring
Development of Fetal Monitoring Machines
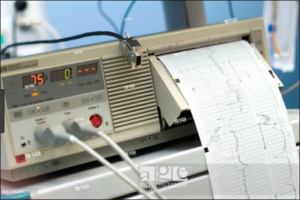 In the late 1960s, electronic equipment was developed that made it possible for a machine to continuously listen and record the activity of the fetal heart, as well as tracking the frequency and length of labor contractions.
In the late 1960s, electronic equipment was developed that made it possible for a machine to continuously listen and record the activity of the fetal heart, as well as tracking the frequency and length of labor contractions.
EFM was originally designed to monitor the unborn babies of women with very serious medical diseases, high-risk pregnancies, and women who developed serious complications during labor.
The malpractice crisis of the mid-1970s changes everything
An unexpected, and in many ways irrelevant event — the malpractice crisis of 1975 — changed the way this technology was used in the US. Due to several unexpectedly large malpractice settlements, the companies that sold professional liability insurance dramatically increased their premiums. This provided a great hue and cry from the medical community and made the costs associated with malpractice insurance the topic of newspaper headlines for several weeks. Following this focus on litigation, there was a 6-fold increase in the use of continuous EFM in hospitals all across the country.
As more and more hospitals routinely used continuous EFM for all their labor patients, EFM was formally adopted as the standard of care in American hospitals. No long a special protocol reserved for women with serious medical complications and/or a very high-risk pregnancy, continuous EFM was used on all laboring women, no matter how healthy the mother or low risk her pregnancy.
The No 1 obstetrical procedure in the US is continuous Electronic Fetal Monitoring
According to an article published in April of 2011 by a practicing obstetrician:
“ . . . intrapartum fetal heart rate monitoring is the most common obstetric procedure performed in the United States.
Despite the widespread use of EFM, there has been no decrease in cerebral palsy. … trials show that EFM has no effect in perinatal mortality or pediatric neurologic morbidity. {1}
Citation #1. “Heart Rate Monitoring Update”
The Female Patient, April 2011
In hospitals, the hourly reimbursement rate for continuous electronic fetal monitoring by many health insurance companies is several hundred dollars an hour, in some cases as much as $400. The routine use of this expensive technology, along with a significant increase in Cesarean surgeries associated with the routine use of c-EFM, is an economic double whammy that has contributed significantly to the high and continuously rising cost of childbirth services in the US over the last 50 years.
This is particularly an issue for larger hospitals that have central monitoring systems. In these hospitals, L&D nurses and obstetricians sit at the Nurses’ Station in the hallway and watch banks of computer screens simultaneously displaying the EFM tracing from several different labor rooms. Hospitals with central monitoring have an even higher C-section rate than those where monitoring the electronic monitor display is the direct responsibility of the L&D nurse assigned to that patient.
The universal use of c-EFM continues to make childbirth services disproportionately expensive in the US. In parts of the country, hospitalization for childbirth is approaching, and in some cases equals the cost of an organ transplant (over $100,000).
 The obstetrical profession’s mistaken belief that not using continuous EFM equates to malpractice
The obstetrical profession’s mistaken belief that not using continuous EFM equates to malpractice
As expert witnesses, obstetricians are frequently called on to testify in legal cases about electronic monitoring. As spokesmen for the obstetrical profession, they also funnel information to the news media about the role of EFM.
A majority of obstetricians spokesmen believe that any failure to utilize this potent combination of continuous EFM and nearly-instant access to Cesarean delivery for all childbearing women, no matter how healthy the mother or normal the pregnancy constitutes substandard or negligent care.
In the opinion of these individuals, this constitutes medical malpractice if the provider is a hospital or physician, and criminal neglect or the “earliest form of child abuse” if the decision to not be electronically monitored during labor is made by the parents or a midwife. While these opinions come from highly regarded professionals, they are nonetheless devoid of scientific support, untrue, and misleading in the extreme.

Based on a consensus of the scientific literature, the truly informative statement — the type of information legally required as part of the “informed consent” process, is that continuous EFM is NOT recommended when the mother-to-be is healthy and her pregnancy is normal.
Furthermore, a professionally licensed maternity care provider would be legally obliged to inform healthy childbearing women that auscultation protocols are the science-based ‘best’ choice, and that c-EFM is actually contra-indicated, that provide no benefit while introduces unnecessary risks and unproductive expense.
The Future of Maternity Care in the United States
A new vocabulary, a new perspective, a new way to provide care during pregnancy and childbirth
The basic purpose of maternity care for healthy women with normal pregnancies is to protect and preserve the health of these already healthy women. The needs of healthy women are fundamentally different than those of women with serious complications and high-risk pregnancies. Maternity care is a different discipline, with a perspective very different from that of obstetrics, which is a surgical specialty.
It would be enormously helpful if we used a different vocabulary to distinguish and discuss this functional distinction, identifying maternity care as professional discipline focused on healthy childbearing, while obstetrics would continue to be recognized as the surgical specialty that it is, a discipline that focuses on the diseases and abnormal conditions of female reproductive biology, complications of pregnancy and management childbirth in women who have high-risk pregnancies or develop complications during labor, birth or postpartum period.
Relative to this 70-85% childbearing population, the goal for our healthcare system must be a cost-effective model that is able to preserve health of already healthy women and effectively prevent, or successfully treat, minor complications that arise during pregnancy and childbirth and in case of a serious complication, consult with, refer or transfer of care to high-risk obstetrical specialists.
What we need as individuals, as childbearing families and as a society is to be certain that all customary childbirth practices are scientifically sound, including the protocols for fetal monitoring used when providing childbirth services to healthy women with low-risk pregnancies. This means safe, cost-effective, and also meets the physical, social and emotional needs of childbearing families and their newborn babies.
Mastery in normal childbirth services for healthy women with normal pregnancies means bringing about a good outcome without introducing any unnecessary harm or unproductive expense.
The ideal maternity care system seeks out the point of balance where the skillful use of physiologically-based care, and adroit use medical interventions whenever necessary, results in the best outcome with the fewest number of medical/surgical procedures and least expense to the health care system.
 Ultimately, the quality of maternity care must be is judged by its results — the number of mothers and babies who graduate from its ministration as healthy, or healthier, than when they started.
Ultimately, the quality of maternity care must be is judged by its results — the number of mothers and babies who graduate from its ministration as healthy, or healthier, than when they started.
As the #1 obstetrical procedure in the United States — one that is uniquely expensive for those who pays these bills (including federal MediCaid program — we need to be sure that EFM does what its manufacturers say it does.
Based on the current consensus of the scientific literature amassed over the last 40-plus years, the “best practices” as defined by best outcomes for mothers and babies and least expense to the society both in money and human terms must be scientifically identified and implemented as the legal and ethical standard of care for healthy women with normal pregnancies who decline routine interventions during labor unless they become medically necessary.
Providing maternity care to healthy childbearing families
 If obstetrics, for whatever reason, is not configured to meet the real needs of childbearing women, then it must systematically reform itself. If unwilling or unable to do this, the obstetrical profession can and should change its focus by reclaiming its historic role as a doctor trained in a speciality to meet the needs of women suffering from diseases and pathological conditions associated with their reproductive biology, including hormonal issues, infertility, cysts, tumors, and complications of pregnancy, childbirth and the postpartum period.
If obstetrics, for whatever reason, is not configured to meet the real needs of childbearing women, then it must systematically reform itself. If unwilling or unable to do this, the obstetrical profession can and should change its focus by reclaiming its historic role as a doctor trained in a speciality to meet the needs of women suffering from diseases and pathological conditions associated with their reproductive biology, including hormonal issues, infertility, cysts, tumors, and complications of pregnancy, childbirth and the postpartum period.
In this context, it’s appropriate to stress how obstetrics as a surgical discipline differs from the basic purpose of maternity care — to protect and preserve the health of already healthy women.
Its a function of the health care system to create a cost-effective model of maternity care that is able to preserve health and effectively prevent or successfully treat non-surgical complications during pregnancy and childbirth.
This factors in the full spectrum of reproductive mortality and morbidity over the course of a woman’s entire reproductive life, including delayed and downstream problems, complications in subsequent pregnancies, future fetal or neonatal loss and the overall cost of care to individuals and society.
It is for this reason that continued routine use of EFM on healthy women with normal low-risk pregnancies cannot be permitted to continue.
 The scientific evidence is overwhelming — routine EFM resulting in a sharply elevated Cesarean rate without any benefit to the mother or baby. Cesarean deliveries needlessly expose childbearing women to all the intra-operative complications of major surgery, a 13-fold increase in emergency hysterectomies within 14 days of the Cesarean birth, secondary infertility, and potentially fatal complication for both mothers and unborn/newborn babies in subsequent pregnancies.
The scientific evidence is overwhelming — routine EFM resulting in a sharply elevated Cesarean rate without any benefit to the mother or baby. Cesarean deliveries needlessly expose childbearing women to all the intra-operative complications of major surgery, a 13-fold increase in emergency hysterectomies within 14 days of the Cesarean birth, secondary infertility, and potentially fatal complication for both mothers and unborn/newborn babies in subsequent pregnancies.
The following series will address the why, when, how of both EFM and auscultation, including the diverse circumstances of their use and their cost in financial and human terms, the scientific literature and Action Plan to correct one of its most serious problems, which is the routine use of an obstetrical procedure — continuous EFM — which was designed to be used in very high risk pregnancies but instead has been allowed by the medical profession and the public to become a universal standard of care used during the normal labors of healthy women with low-risk pregnancies.
faith gibson, LM ^O^
 Former L&D nurse, California licensed professional midwife #41, author-editor of the California College of Midwives’ Standard of Care (2004); appointed to the Medical Board of California’s Midwifery Advisory Council, served 6 years, 3 as its first Chair (2007-2013); web-wife to 8 midwifery and childbirth-related websites
Former L&D nurse, California licensed professional midwife #41, author-editor of the California College of Midwives’ Standard of Care (2004); appointed to the Medical Board of California’s Midwifery Advisory Council, served 6 years, 3 as its first Chair (2007-2013); web-wife to 8 midwifery and childbirth-related websites
Favorite Publication: Time Traveler’s Perspective on Normal Childbirth published in the journal BIRTH in September 2011
BIRTH-PracPerspective_MyArticle_Sept11_2011
Continue to Part 1A ~ Fetal Monitoring ~21st-century Conundrum for the US


