Editor’s Note:
This is the very last post in this series. However it is followed by peer-reviewed studies (full text or substantial excerpts) cited in the Mayday series and essays based on the scientific literature by practicing obstetricians. Please read them as well.
The disappointing choice by the obstetrical community to focus on obstetrical technology instead of the well-being of healthy childbearing women
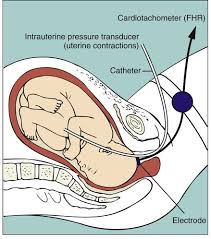
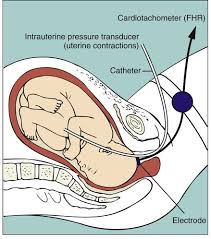 In the 1970s, continuous electronic fetal monitoring (EFM) was introduced as a reliable technology that would help obstetrical provider diagnose fetal hypoxia in time to prevent neurologic damage to the fetus. By the early 1990s, more than 75 percent of the nation’s birth attendants had switched from intermittent auscultation to EFM. In real life terms, this expensive, complex, and off-putting technology replaced the simple act of listening to the unborn baby’s heart rate on a regular schedule (i.e. auscultation) by a living, breathing human being that and talked to the mother.
In the 1970s, continuous electronic fetal monitoring (EFM) was introduced as a reliable technology that would help obstetrical provider diagnose fetal hypoxia in time to prevent neurologic damage to the fetus. By the early 1990s, more than 75 percent of the nation’s birth attendants had switched from intermittent auscultation to EFM. In real life terms, this expensive, complex, and off-putting technology replaced the simple act of listening to the unborn baby’s heart rate on a regular schedule (i.e. auscultation) by a living, breathing human being that and talked to the mother.
Since then EFM has been the de facto standard for obstetrical care in the US. However, there never has been a scientifically validated foundation for the claim that continuous EFM would dramatically reduce, if not altogether eliminate, cerebral palsy and other permanent neurologic disabilities.electronic fetal monitoring.
However, multiple studies identified the use of EFM provided NO benefit to on healthy childbearing women or their unborn baby. Nonetheless, EFM leads strapped to the laboring woman’s abdomen tethered her to her bed
As noted in the many studies quoted above, the universal use of EFM did not turn out to be the answer to the obstetrician’s prayer to eliminate cerebral palsy, neonatal encephalopathies and perinatal mortality as everyone hoped.
But this disappointment did nothing to dislodge obstetrical faith in electronic monitoring systems. The profession spent its a huge proportion of its resources trying to improve and refine EFM’s electronic circuitry and making other tweaks the machinery, alway anticipating that the perfected ‘magic bullet’ was just around corner.
Unfortunately, this blind faith in the ability of c-EFM to eliminate newborn neurological complications created a series of problems, not the least of which was a malpractice nightmare for obstetricians. Having extolled the virtues of obstetrical care augmented by c-EFM and Cesareans as a virtual guarantee of a ‘perfect’ baby every time actually set up a situation in which obstetricians got sued every time they didn’t deliver “the goods” — i.e. a perfect baby.
But the bigger picture is even more of an issue for childbearing families and for society. The obstetrical profession’s fifty-year focus on refining and expanding the EFM system diverted attention away from studies that looked into other origins and explanations for the unexpected problems of cerebral palsy and neurologically-damaged babies subsequent to perfectly normal pregnancies and normal labors and births.
Why the subtle distinction btw acidemia & hypoxia matters
The distinction btw metabolic acidosis and labor-related hypoxia is subtle even for highly-trained medical professionals. But this is critically important, as the reasoning behind c-EFM was the assumption that fetal hypoxia during labor was the causative agent in cerebral palsy and similar neurological problems.
Continuous EFM was specifically developed to detect the slow development of hypoxia over long periods as the unborn baby was being exposed to less-than-adequate oxygenation (such as a placental insufficiency, post-mature pregnancy or maternal hypertension).
The other known cause for CP and neonatal encephalopathies are of course acute obstetrical emergencies, such as a placental abruption, cord prolapse or a life-threatening medical emergency for the mother. But again, these emergency have little or nothing to do with EFM, as they are usually diagnosed by other symptoms and monitoring the vital signs of the mother. No form of EFM, no matter how well ‘perfected’, can predict, prevent or treat these occurrences.
In acute intrapartum emergencies, anoxia (the most severe type of hypoxia) is terribly damaging to the unborn baby. But all and all, this type of intrapartum emergency is rare; we know because the use of c-EFM hasn’t eliminated them. However, the depressingly stable rate of CP hasn’t budged over the last 50 years in spite of c-EFM. Along with newer research, this tell us that pre-labor metabolic acidosis is the stubborn cause of 92% of all CP cases and other neurological problems not related to an intra-partum emergency.
If you are interested in learning how intermittent auscultations (IA) works, this link will take you to a stand-alone post on IA
Conclusion
As long as this essay is, I didn’t include many issues known to increase the problems associated with our highly-medicalized obstetric system.
The topic that got the short shift was the simple but profoundly important principles of physiological management. Physiologic methods aim to safely manage childbirth without depending on drugs like Pitocin to progress the labor, narcotics to manage pain, or surgical procedures to deliver the baby.
Instead of obstetrical interventions, midwives depend on the normal physiology of childbearing, which in turn depends on mothers being able to move around freely, receive one-on-one support, able to use upright positions and make right use of gravity, as well as non-drug methods of pain relief that include walking, hot showers, and submersion in a deep water tub.
Midwives believe in the innate ability of childbearing women to labor spontaneously, push their babies out under their own power and properly take credit for this accomplishment.
As midwives, we do our part by fully present throughout active labor, eyes-on, ears-on, hands-on care and generous frequent encouragement. This includes but is not limited to monitoring the physical wellbeing of the mother, and intermittent auscultation (IA) of the fetus, to be as sure as possible that we would detect any problems for the unborn baby and take appropriate action.
Contrast this with allopathic medicine, which is officially defined as the use of drugs, surgery and ionizing radiation. American MDs are not interested in learning about ways to do things that don’t include the use of drugs or surgery. As a result, our medical schools don’t teach the physiological management of normal childbirth. Practicing obstetricians generally don’t know, don’t use, don’t like, don’t understand, don’t believe in and certainly don’t approved of physiologically-based care or practitioners (i.e. midwives) who use provide physiological management.
So it comes as no surprise that over 90% of women laboring in the obstetrical system are given epidural and are continually monitored. The blow-back from this creates a consistent set of other problems that require the same few interventions — IV Pitocin to speed up the labor, maternal oxygen mask as minor but non-reassuring changes begin to show up on EFM strip and far too often, the decision to do an emergent c-section based on a combination of slow or no progress and increasing signs of possible fetal distress as recorded by the EFM (i.e. non-reassuring fetal heart rate).
 The Glaringly Obvious Effect of EFM — turning healthy women into passive & bed-ridden maternity patients
The Glaringly Obvious Effect of EFM — turning healthy women into passive & bed-ridden maternity patients
What stick out most in my mind as I googled photos of electronic fetal monitors and laboring women as was how EFM turned healthy women into passive maternity patients, lying still and listless in bed, so as not to infer with working of the the machines they were hooked up.
 Everything about the design of ‘modern’ obstetrical units and the ministrations of the L&D staff revolves around the hospital’s computer-based electronic fetal monitoring system. The nurses have to keep graph paper in the tray, unplug all the leads every time the mother has to go to the bathroom, and most time-consuming of all, repeatedly tweak the placement of the toco and monitor belts on the mother’s belly find the signal and be sure its being is recorded.
Everything about the design of ‘modern’ obstetrical units and the ministrations of the L&D staff revolves around the hospital’s computer-based electronic fetal monitoring system. The nurses have to keep graph paper in the tray, unplug all the leads every time the mother has to go to the bathroom, and most time-consuming of all, repeatedly tweak the placement of the toco and monitor belts on the mother’s belly find the signal and be sure its being is recorded.
Everyone hopes that EFM tracing will keep the doctors and the hospital from being sued and the icy fear in the back of their mind that they might slip up and the EFM proof needed to prevent litigation can’t be found.
 But the real tragedy is what c-EFM does to laboring women. They have been ‘disappeared’ from the system. Instead of healthy individuals experiencing the most important and joyous day of their lives, they have been dependably turned into faceless compliant patients doing their part to make the OB department into a profit center for the hospital, while their unborn fetuses are the stars of the show.
But the real tragedy is what c-EFM does to laboring women. They have been ‘disappeared’ from the system. Instead of healthy individuals experiencing the most important and joyous day of their lives, they have been dependably turned into faceless compliant patients doing their part to make the OB department into a profit center for the hospital, while their unborn fetuses are the stars of the show.
 Teaching illustration and teaching mannequins portray the mother-to-be a faceless vessel for the fetus, with little or no importance of her own.
Teaching illustration and teaching mannequins portray the mother-to-be a faceless vessel for the fetus, with little or no importance of her own.

