Overview & Chapter 1
~ The disturbing story of obstetrics in America from 1910 to 1980 and why that still matters in 2023 ~
Unless you are pregnant, it’s unlikely you’d that have any natural interest in either the history or contemporary practice of obstetrics. Nonetheless, there are two very good and very contemporary reasons for every American adult to know about the historic and the modern-day practice of obstetrics in the United States. How obstetricians conduct childbirth in American hospitals is is dramatically different than the historic role of obstetrics in most other countries, which was and still is to treat complications.
Why decisions made during this historic period still matter today

From 1910 to 1980, childbirth in America was a surgical procedure that included chloroform anesthesia, the use of forceps to extract the baby from the mother’s unconscious body and stillbirth of severely depressed babies not able to breathe on their own after being born.
The reason this historic period still matters today is that the basic philosophy of obstetrics as it was developed 1910 is still at the core of its contemporary practice. Beginning in the early 20th century, influential leaders in American obstetrics believed the unpredictable dangers sometimes associated with childbirth could be prevented by pre-emptively (rotuniely) using medical interventions and conducting childbirth as a series of surgical procedures.
Quote published by 1911 Dr.Emmons, MD: Obstetrics Care in the Congested Districts of our Large American Cities
Unfortunately, their confidence in this “proactive” strategy was misplaced, as these very interventions increased the rate of complications. Methods used to make childbirth safer in actual fact made it more dangerous and increased the number of mothers and babies harmed by a process that was meant to help them. As a result, the United States has the third highest maternal mortality rate in the industrialized world.
Nonetheless, this same underlying philosophy — the prevention of complications via the “pre-emptive strike” — still defines the practice of obstetrics in 2023. the specific interventions being used are different than those used in 1910, but interventions used to make childbirth safer are still making it more dangerous, and also are very disruptive to the mother’s experience of labor.
While the idea of “safer” still includes the well-being of both mother and baby, the focus on “safety” since the infamous “malpractice insurance crisis of 1976 has been protecting obstetricians from lawsuits. This is a primary factor underlying the routine use of elective inductions, continuous electronic fetal monitoring (EFM), Pitocin IVs to speed up labor, and liberal use of Cesarean surgery any time the EFM strip is something other than “perfect”.
As a result, the United States has gone from third place in the rate of mothers dying as a result of childbirth to first place. As of this publication, the United States has the very highest maternal mortality rate of all developed countries. In fact were are 128th place, between the third-world countries of
If you are woman of childbearing age, a mother with daughters and granddaughters, or the father, brother, husband or son of childbearing women, then information about the historic and contemporary obstetrics in America is a matter of life and death. For the entire 20th century, the United States has had a disproportionately high maternal mortality rate compared to other industrialized countries. Unlike the integrated midwifery systems used in Europe that support the natural biology of childbirth, obstetrics the United States developed as surgical specialty. The style of care provided used many medical and surgical interventions on healthy childbearing.
For healthy women with normal pregnancies, obstetrical interventions were far more dangerous than the supportive and non-interventive care provided by general practitioners and professional midwives. The reason for this dramatic departure from traditionally supportive practices was that American obstetricians, unlike their peers in other developed countries, believed that the “normal” biology of human childbirth was actually a dangerously pathological process. Obstetrician were convinced they had a professional duty to correct Mother Nature’s “mistakes” in order to make childbirth safer.
Starting in 1910, the new obstetrical “standard” included the routine use of medical and surgical interventions during labor and birth in healthy women with normal pregnancies. This included separating women from their family and sequestering her behind the closed doors of labor ward that read “No Admittance Authorized Personnel Only” in big black letters. Every labor patient was given large and frequently repeated injections of “Twilight Sleep” drugs — a strong narcotic (oriignally morphine, later replaced by Demeral) mixed with the mind-altering drugs scopolamine.
Unfortunately, a considerable number of laboring women had a paradoxical reaction to the drug scopolamine. Instead of slipping into a very deep sleep, the drug incited a state of panic. They tried to stand up in the bed or crawl out over the bed rails. When the nurses tried to keep them from falling out of bed, they would often hit or bite the nurse. As a result, these labor patients had to be “restrained”.
Some hospitals use a modified “straight jacked” that strapped them to the bed. The policy at our hospital in the 1970s was to put these labor patients in “four-point” restraints. This consisted of using the large leather wrist and ankle restraints from the hospital’s psychiatric ward. These were to put on wrists and ankles of the labor patient and then attached to the four corners of her labor bed. This forced the woman to lay flat on her back for the entirety of the labor, which could be more than 24 hours.
When the patient’s labor advanced to the pushing stage, she would be taken by stretcher to delivery room — an obstetrically outfitted operating room. Normal childbirth was conducted as surgical procedure that began by rendered the mother-to-be was unconscious under general anesthesia. “Delivery” was a series of surgical procedures. This began with the doctor cutting and episiotomy, and asking the nurse to provide fundal pressure. This pressed the unborn baby deeper into the mother’s pelvis and helped the doctor extract the baby with forceps. Then the doctor manually removed the placenta, This required him to put on a special type of sterile glove with a cuff that came up to his elbow. Then he inserted his hand into the mother’s vagina by inserting and suturing of the episiotomy incision.
This was happening decades before the discovery of antibiotic, when there was no effective way to treat potentially fatal infections. Unfortunately, the new American standard of care was disastrous childbearing women.
For the first half of the 20th century, two million women gave birth each year. During the period of 1900 to 1937, there was one maternal death out of every 80 live births. Between 1916 and 1925, the annual MMR rate rose to 25,000. From 1900 to 1930, a total of 460,000 maternal deaths calculated on the childbearing population (ages 16 to 45).
Successful efforts by the obstetrical profession to criminalizes and eliminate midwives
At the beginning of the 20th century (1900) the ratio of births attended by midwives and MDs was about fifty-fifty. However, doctors in general were very critical of midwives, resented the economic competetion they resented and believed that they were all untrained and therefore dangerous.
1906 ~ Dr. Gerwin
“…. the typical, old, gin-fingering, guzzling midwife, … her mouth full of snuff, her fingers full of dirt and her brain full of arrogance and superstition”
1907 ~ Dr. Mabbott: … “un-American”
Drs. Emmons and Huntington: “the overconfidence of half-knowledge, …unprincipled and callous for the welfare of her patients”
In 1907 in the state of Massachusetts, influential leaders of the obstetrical profession were able to get a state law passed making it illegal for midwives to attend births. This was soon followed by laws criminalizing midwives in other states.
The appropation that doctors visited on midwives was staggering — the word “midwife” became the equivalent of the “n”word in the vocabulary in America:
1911 Arthur Brewster Emmons, 2d, M.D., Boston and James Lincoln Huntington, M.D., Boston.
“The history of temporizing with the ignorant, half-trained, often malicious midwife in our sister states to-day reads like many another misguided “freedom ” which is virtually a license by the state to practice quackery on an ignorant, unsuspecting public. The women and infants pay for this “freedom” in deaths, unnecessary invalidism and blindness.”
The philosophy of the obstetrical profession in the United States was succinctly expressed in this 1911 publication in the Boston Medical and Surgical Journal, 02-23-1911, page 261 {*}
“… we believe it to be the duty and privilege of the obstetricians of our country to safeguard the mother and child in the dangers of childbirth.
The obstetricians are the final authority to set the standard and lead the way to safety. They alone can properly educate the medical profession, the legislators and the public.”
A Review of the Midwife Situation ~ by Arthur Brewster Emmons, 2d, M.D., Boston and James Lincoln Huntington, M.D., Boston.
Obviously this was as very successful strategy, as the ratio of midwife-attended births fell from 40 to 60% to just 13% by 1920s. The only midwives allowed to continue practicing were Black “granny” midwives in the South that attended births of blacks mothers and immigrants. But even this concession was just a pragmatic convenience, since segregated white hospitals did not provide care to Afro-American patients under any circumstance.
The statistical connection between the increasing maternal mortality rate and the suppression and eventual abolition of midwives
Unfortunately, the disproportionately high maternal mortality rates were not kind to the budding obstetrical profession. The more obstetricians were successful in criminalizing and eliminating midwives, while medical schools were frantically pumping out more and more new graduates to replace them, the higher the rate of women dying from childbirth-related causes.
Despite the best efforts of doctors to intervene more often and earlier in the labor an effort to stem this tide, it unexplainably continued to rise at a very alarming rate. However, the historical record make the supposedly “inexplicable” very plain — eliminating access to the non-interventive care of midwives and replacing it with an ascending rate of medical interventions and surgical procedures such as forceps deliveries and manual removal of the placenta turned normal birth into a death sentence for healthy childbearing women.
1911 ~ Dr. Ira Wile, MD, New York City
“In NYC, … death from puerperal sepsis occur more frequently in the practice of physicians than from the work of the midwives. [1911-G TAASPIM, p.246, 1911]”
1911~ Dr J. Whitridge Williams, chief of obstetrics, Johns Hopkins, author Williams Obstetrics
1911 ~ Dr. Emmons, MD: “Obstetrics Care in the Congested Districts of our Large American Cities”
“I should like to emphasize what may be called the negative side of the midwife. Dr. Edgar states that the teaching material in New York is taxed to the utmost. The 50,000 cases delivered by midwives are not available for this purpose (i.e. the clinical training of doctors).”
1921 ~ Dr. Levy examined birth-related mortality in Newark, NJ and found a similar relationship to that of Van Ingen’s survey of Manhattan (a 1913 entry above).
|
Birth Attendant: |
Midwife/Home |
Phys/Home |
Hospital |
|
Birth percentage |
38% |
30% |
31% |
|
Maternal Deaths: |
13% |
34% |
52% |
|
Neonatal MR/1000 |
32% |
40% |
34% |
1925 ~ Dr Hardin, MD
It should be mentioned however that the US had the worst maternal-infant mortality of any country in the developed world, except for Brazil.
..in 1921 the maternal death rate for our country was higher than that of every foreign country for which we have statistics, except that of Belgium and Chile.”
… according to [Dr.] Howard maternal mortality in the [US], when compared with certain other countries, notably England, Wales and Sweden is appallingly high and probably unequaled in modern times in any civilized country.
Twenty five thousand women die in the United States every year from direct and indirect effects of pregnancy and labor
… 3 to 5% of all children die during delivery and thousands of them are crippled. [1925-A p. 347 & 350]
1926 ~ Dr. Woodbury
When the Massachusetts Supreme Court (Hanna Porn v. Commonwealth) declared midwifery to be an illegal practice of medicine in 1907, the state’s maternal mortality was 4.7 per 1000 live birth.
By 1913 it had risen to 5.6 and by 1920 it was up to 7.4
1931 ~ A report published by the White House Conference on Child Health and Protection by the Committee on Prenatal and Maternal Care, noting the wide disparity between safe care provided by midwives and the highly risky care of many physicians.
The report’s physician-authors concluded that the care of midwives was safer than the care of MDs, saying that:
“... that untrained midwives approach and trained midwives surpass the record of physicians in normal deliveries has been ascribed to several factors. (emphasis in original)
Chief among these is the fact that the circumstances of modern practice induce many physicians to employ procedures which are calculated to hasten delivery, but which sometimes result in harm to mother and child.
On her part, the midwife is not permitted to and does not employ such procedures. She waits patiently and lets nature take its course.”
1933 ~ Study by the New York Academy of Medicine of 2,041 maternal deaths in physician-attended childbirth*
The investigators were appalled to find that many physicians simply didn’t know what they were doing: they missed clear signs of hemorrhagic shock and other treatable conditions, violated basic antiseptic standards, tore and infected women with misapplied forceps.
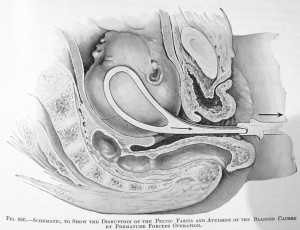
In order to follow the natural 60-degree curve of the pelvis, the obstetrician has to pull up, towards the ceiling to delivery the baby’s head |
At least two-thirds [of the maternal deaths], the investigators found, were preventable. … newborn deaths from birth injuries had actually increased.
Hospital care brought no advantages; mothers were better off delivering at home. … Doctors may have had the right tools, but midwives without them did better. [reported by Dr. Atul Gawande*in his 2006 New Yorker article “The Score“]
1934 ~ The Committee on Maternal Welfare of the Philadelphia County Medical Society
…. expressed concern over the rate of deaths of infants from birth injuries increased 62% from 1920 to 1929. This was simultaneous with the decline of midwife-attended birth and the increase in routine obstetrical interventions, due in part to the influence of operative deliveries.
Excerpt, Dr. Neal DeVitt, MD, a 1975 doctoral thesis: “The Elimination of Midwifery in the United States — 1900 through 1935
1937 ~ obstetrician and famous philanthropist Dr. Alan Guttmacher (associate professor of obstetrics, John Hopkins Hospital) from his book “Into This Universe”:
Though we cannot make an exact comparison between the maternal mortality in the United States and that in European countries, we can at least make a rough comparison.
All who have studied the problem agree that the rate [of good outcomes] for Holland, Norway, Sweden, Denmark is far superior to our own. Why? … it must be due to … the patients themselves and differences in the way that pregnancy and labor are conducted in the two regions.
What about the conduct of labor in the two regions? Here is where the major differences lie. In the first place, … at least 10 percent of labors in this country are terminated by operation. In the New York Report 20 percent of the deliveries were operative, with a death rate of more that 1 in each 100 of the operated, and 1 in 500 of those who delivered spontaneously.
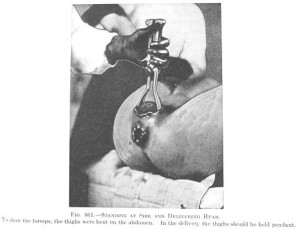
| Very depressed baby, likely from narcotics during labor & general anesthesia during birth Note –> umbilical cord is empty of blood and not pulsing @ the time of the birth |
 |
Let us compare the operative rates of these relatively dangerous countries (USA, Scotland) with those of the countries which are safer. In Sweden the [operative] interference rate is 3.2 percent, in Denmark it is 4.5, while in Holland ….. it is under 1 percent.
What is responsible for this vast difference in operative rates? … Analgesics [narcotic drugs] and anesthetics, which unquestionably retard labor and increase the necessity for operative interference, are almost never used by them in normal cases; and more than 90 percent of their deliveries are done by midwives unassisted.
And midwives are trained to look upon birth as a natural functions which rarely requires artificial aid from steel or brawn.
[1937-A,p. 133-134]
@@ current edit line @ Aug 2023 @
By contrast, maternal deaths in Sweden and neighboring Scandinavian countries were , which used a system of professionally-trained midwives n up by general practitioners and hospital transfer when needed
Equally important is knowing that the childbirth services currently provided by the staff of obstetrical departments of American hospitals to healthy childbearing women continue to include medically unnecessary interventions and surgical procedures that make childbirth unnecessarily dangerous.
From 1950 to 2020, the number rose to 4 million. women gave birth each year maternal mortality rate was deaths
Reasons#1: In general, we Americans just assume the US as the best of everything, which would mean that the US has the very best maternity care system in the Western hemisphere. I wish that was the case, but actually the US has the very highest maternal mortality rate of any developed country (multiple ref incl Commonwealth Foundation, 2022) , and that was BC — Before Covid. Since then our already high rate increased by a third.
Reason #2 In addition to a high level of preventable maternal deaths, American obstetrics is twice (or more) as expensive other developed countries because:
(a) obstetrics is a surgical specialty and obstetricians are not trained to support the normal physiological process of labor; in
(b) American obstetricians routinely intervene When obstetrical interventions developed to treat serious complications of childbirth are routinely used in the labors or what I describe as the “wrong use” of obstetrics on healthy women with normal pregnancies that neither need or want interventions and invasives procedures. Early in the 20th century, American obstetrics, which declared itself to be a surgical speciality, developed a standard of care
In the last two decades of the 20th century, the routine use of electronic fetal monitoring (EFM), Pitocin IVs as a way to induce or speed up labor, and the very “liberal” use of Cesarean surgery.
in the labor and births of healthy women normal term pregnancies.
o know about and understand how should be our modern obstetrical system is founded on a system of obstetrical intervention configured in the first half of the 20th century of providing care for childbirth to the four million or so women that give birth every year in the United States. But Americans generally believe that an important the very unique way that obstetrics developed in the United States to b the matters is that it dramatically altered
In 1910, American obstetricians viewed the normal biology of childbirth in human females as a basically defective and dangerous process. They believed it was their professional duty to correct Mother Nature’s “mistake” and that the best way to do that was by preemptively intervening in childbirth as a ‘standard practice’.
Edit ling –> By routinely using intervention best characterized as what . in all labor by using and birth
purposefully turned healthy women into the patients of a surgical specialty and normal childbirth into a surgical procedure.
While the intentions of the obstetrical profession
This was the most profound change in childbirth practices in the history of the human species.
What happened is that the normal biology of childbirth in healthy women was replaced by a system of routine obstetrical interventions. This redefined “normal birth” from something the mother did — that is, to gave birth under her own power, and be able to take credit for all her hard work — into a series of invasive surgical procedures that the obstetricians did to the mother’s inert body after being rendered unconscious with chloroform anesthesia.
At one point, this massively invasive form of obstetrical care in America resulted in a maternal mortality rate that was 2 to 5 times higher than in developed countries in Western Europe. In a single year (1925) there were an astonishing 25,000 maternal deaths in the United States out of an annual birth rate of 2 million, or a ratio of one maternal death for every 80 live births. Between 1916 and 1925, the rate of
This was in contrast to Europe, which historically had a midwifery-centric system. Midwives professionally-trained in state-run schools attended all normal spontaneous births with a general practitioner available as back up. While the US had one maternal death out of every 80 lives births, the ratio of maternal deaths in Sweden at was one out of 431 births, or more than five times safer. By giving midwives and doctors complementary (instead of competing) roles, maternity care for Swedish mothers was more than five times safer than mothers living in the United States.
But unfortunately, the American obstetrical profession has always seen midwives as economic competition. One of its early PR slogans was “Always a doctor, never a midwife“. Instead of creating “complementary” roles, the goal of the obstetrical profession as carried out by their lobby (the American College of Obstetricians or ACOG) and the goal has always been the total elimination of midwifery in the United States.
The story of why, what, and how American obstetricians imposed an extremely dangerous system of interventive care on healthy childbearing women is both lengthy and complicated. Worse yet, this ethically disturbing and extremely depressing model of unnecessary and risky obstetrical intervention it isn’t over!
Modern obstetrics in America just replaced older forms of interventions and surgical procedures for newer ones during the late 1970s and early 1980s. Unfortunately, the post-1980s story is just as problematic but that is posted elsewhere on this website.
The story begins — why, what, and how
It pains me to write this, but the 12-point bulleted paragraph below describes what was done in simplified language. This also includes the why — the obstetrical profession’s motives, goals, economic issues interventionist policies and the politicized practices of hospital-based obstetrics.
In 1910, the American obstetrical profession began promoting a highly interventive model of obstetrics as the new American “standard of care” for normal childbirth. While the specific interventions changes — Twilight Sleep drugs (morphine and scopolamine) were replaced with Demerol, the new drug “Pitocin” became available to induce or speed up labor, and forceps deliveries were replaced by Cesareans. However, the obstetrical model was always to do “something” other than wait patiently and provide active hands-on support that help the laboring woman to progress and give and give birth spontaneously.
Here is a rather lengthy list of the historical issues that i describe as the “wrong use of obstetrics”. Unfortunately, the built-in drive to intervene still underlies the practice of obstetrics in the United States.
- To distinguish American obstetrics as separate and distinct from midwifery, they declared that obstetrics in the US, unlike its European counterparts, was a new brand surgical specialty and that normal childbirth was now considered to be a surgical procedure
- To eliminate what they saw as “illegitimate” competition between obstetricians and inferior “female practitioners” (i.e. midwives), they declared themselves, as MDs, to henceforth have a legal monopoly over all forms of pregnancy and childbirth services
- Over time this newly-elevated status allowed the obstetrical profession to greatly increase the income of doctors who attended births
- They legally categorized childbirth in middle- and upper-class (white) women to be a pathophysiology, and publicly described sexual reproduction in this class of human females to be “a nine-month disease that required a surgical cure”
- After defining normal childbirth as a pathological process in middle- and upper-class white women, the next logical step was to insist that this economically well-off demographic be electively hospitalized for childbirth
- Because childbirth was defined as a ‘surgical procedure’, the laboring women was isolated in a special “sterilized” ward; husbands and family members were not allowed to stay with or even see their wife during labor or to be present at the baby’s birth
- Normal childbirth as a pathology in this demographic was conducted as a series of medical interventions, starting with routine use of the Twilight Sleep drugs (narcotics and the hallucinogenic and amnesic scopolamine); since these drugs left each labor patient in a semi-conscious stupor, these women were never allowed to get out of bed during labor; sometimes this required the use of the four-point leather wrist and ankle restraints attached to the bed posts
- The birth of the baby was conducted as a series of invasive surgical procedures that began with general anesthesia and included the routine use of obstetrical forceps to compensate for the inability of an unconscious woman lying flat on her back to push effectively; the routine use of forceps was also seen as necessary to maintain the obstetrical provider’s skill in using forceps in emergent situations where they actually became a life-saving procedure
- The elective hospitalization of well-off middle- and upper-class women” during labor, the conduct of the surgical procedure of “delivery”, and the subsequent 14-day “lying-in” period for both mother and baby, created a brand new and highly profitable revenue stream for any hospital that already had or put in new a “lying-in” (i.e. maternity) ward
- Dr J. Whitridge Williams specifically promoted the idea that existing hospitals should add lying-in wards or open a small “lying-in hospital” as a way to generate income to be use to upgrade their facility into a full-service hospital with modern medical technology;
- The routine use of Twilight Sleep drugs and “the delivery” as a surgical procedure done under general anesthesia was a ‘selling point’ to promote the patronage of middle and upper-class “modern” women, whose families could pay for a hospital birth and 14-day postpartum stay for mother and baby
- The new income generated by maternity wards allowed the hospitals to spend money on “capital-intensive” equipment and renovations, such as buying a new x-ray machine, industrial autoclave, and other expensive medical equipment, purchasing microscopes and other equipment for a new clinical laboratory, upgrading its surgical suits with ceramic tile walls and floors, special operating room tables, and powerful overhead electric lights
- Some proportion of these hospitals were able to use the dependable income generated by the healthy women that populated their “lying-in” (i.e. maternity) wards to eventually elevate the status of their institution to that of a “general hospital” that made comprehensive healthcare to available to the population of an entire geographical region by being able to provide “state of the art” services to both genders and all ages that included life-saving diagnostic, emergency, medical, surgical, obstetrical, pediatric in-hospital services
The overview account above describes what was done and why; the first chapter focuses on how these goals were achieved.
 Chapter One ~ The motives behind the obstetrical profession’s 1910 decision to define normal childbirth in healthy upper-class white women to be inherently pathological and its far-reaching consequences
Chapter One ~ The motives behind the obstetrical profession’s 1910 decision to define normal childbirth in healthy upper-class white women to be inherently pathological and its far-reaching consequences
I was first introduced to the highly obstetricalized childbirth practice of American obstetrics in the 1960s. By then, the unquestioned policies and protocols that defined the care of healthy hospitalized childbearing women were already more than a half century old.
When I retired from L&D nursing 13 years later, the obstetrical protocols at a different Florida hospital still included drugging every new labor patient, whether she consented or not, with large and frequently-repeated doses of narcotics, giving the mother general anesthesia, and delivering the baby with forceps. The more things change the more they stay the same.
While our doctors were no longer giving the generic drug scopolamine, it was only because very aggressive pharmaceutical sales reps convinced them that newer and more expensive psychotropic drugs were ‘so much better’. All the other interventions and invasive procedures, from general anesthesia (safer but still explosive gas Cyclopropane), forceps and manually extracting placentas, all continued on as if the 1910 version of interventive obstetrics had become the law of the land.
Our OBs still believed they were doing the mother a big favor by cutting a ‘generous’ episiotomy to prevent “women’s troubles such as incontinence and uterine prolapse. When suturing the episiotomy afterward they paid particular attention to “the husband stitch”. Obstetricians claimed these last few tights stitches would restore “virginal tightness” to the newly-delivered mother’s vagina, the purpose being to keep her husband happy in the marriage bed.
Thankfully this specific historical period organized around racial discrimination and routine use of Twilight Sleeps drugs and general anesthesia for all its white labor patients is long gone. But unfortunately, the dysfunctional nature of interventionist obstetric for healthy women remains generally unchanged.
This is the result of the American obstetrical profession’s century-long refusal to acknowledge the important functional difference between healthy childbirth women with normal pregnancies, who don’t benefit from the routine use of obstetrical interventions, and pregnant women with serious medical conditions, high-risk pregnancies or who develop complications and quit obviously benefit from intensive obstetrical management.
The appropriate and cost-effective model of care for healthy childbearing women with normal pregnancies is physiologically-based (i.e. non-medical) care provided by family practice physicians and professional midwives. That is the system that has been successfully used in most Western European countries for the past 2 centuries but is decidedly not what happened in the United States, starting in 1910!
The lop-sided power dynamics between the obstetrical profession, the nursing staff as hospital employees specifically hired to carry out “Doctor’s Orders”, and the endless stream of laboring women has changed very little over the last half century. The obstetrical profession as a national system continues to treat normal labor in healthy women as a potential emergency and childbirth as safest when conducted as a surgical procedure by an obstetrically-trained surgeon.
For the last half-century, all the efforts of individuals, consumer organizations, professional groups, and hospital nursing staff to end these “business as usual” interventive practices and create a childbearing woman-centered system (rather than doctor-centered) have so far been a dismal failure as obstetricians push for more — not less- interventions.
Currently, that is scheduled inductions of labor or elective C-sections before the baby’s due date!
Unfortunately, obstetrics in American is about obstetricians; it is organized around the needs and wellbeing of obstetricians instead of the needs of the healthy childbearing women that they are supposedly serving.
Healthy childbearing women are still being constrained by harmful policies that result in them being talked into or scared into routine interventions such as elective induction, use of continuous electronic fetal monitoring, and medically-unnecessary interventions and Cesarean surgeries.
Rather than a focus on meeting the biological and psychological needs typical for the majority of healthy labor patients, obstetricians order interventions that speed up or slow down labor, or to have an elective scheduled or “repeat” C-sections.

Many obstetricians also believe these interventions help to protect them and their hospital from malpractice suits, particularly to do repeat C-sections, thus avoiding the risks of a vaginal birth after a previous Cesarean (VBAC).
Unfortunately, this simply substitutes the risks of repeated major abdominal surgery for the risk of VBAC. It turns out that repeat CS are more risky than the first or ‘primary’ Cesarean due to the build-up of additional adhesions after each and every repeat surgeries.
Other find these interventions to be economically advantages, as it allows them to attend more deliveries and gyn surgeries.
However, L&D nurses who carry out these interventions know full well that much of what they are being told to do to labor women is both unnecessary and harmful. Unfortunately, this charade – the idea that the pre-emptive use of obstetrical interventions makes childbirth safer for healthy women – goes on unabated every hour of every day in every hospital obstetrical department all across America.
Click here to continue –> The Big Reveal ~ Motives hidden beneath claims that more obstetrical interventions make childbirth safer for healthy childbearing women