Easy-to-share link ~ https://tinyurl.com/yxfx7d8u
Word count 1300
Conclusion of the Mayday Series ~ Part 1 ~
Be sure to read Acton Plan in Part 2
This series began with big (and embarrassing) questions about the contemporary practice of obstetrics in America.
The most central of all was simply:
“Why has American obstetrics strayed so far from its noble foundations?
 There are many examples, but the specific issue addressed in the Mayday! series is the inappropriate use of continuous electronic fetal monitoring (EFM) as the standard of care for healthy women with normal (low-risk term) pregnancies, which is approximately 70 to 85% of the childbearing populations.
There are many examples, but the specific issue addressed in the Mayday! series is the inappropriate use of continuous electronic fetal monitoring (EFM) as the standard of care for healthy women with normal (low-risk term) pregnancies, which is approximately 70 to 85% of the childbearing populations.
This expensive and complex technology was developed to monitor the labors of women with high-risk pregnancies and complications that were highly risky to unborn babies. For reasons that defy logic, this technology for high-risk pregnancies has become the universal standard for healthy women with low-risk pregnancies.
Fetal Monitoring: the Verb and the Noun
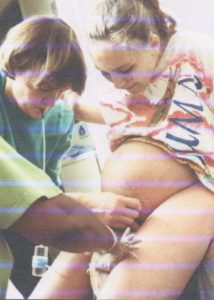
The Verb: It’s a well-documented fact that childbirth outcomes for healthy laboring women and their unborn babies are equally good when L&D nurses, midwives or physicians use a fetoscope or hand-held Doppler to monitor (the verb) the unborn baby during labor.
Actually maternal-baby outcomes for hands-on auscultation are better than c-EFM when the increased C-section rate, complications and unproductive expense associated with routine use of EFM are taken into account.
 This traditional method, which has been used since the early 20th century to determine fetal well-being, is called auscultation.
This traditional method, which has been used since the early 20th century to determine fetal well-being, is called auscultation.
The fetal heart rate is regularly listened to during labor on a schedule that gets increasingly frequent as the contractions become longer, stronger and closer together.
Depending on the stage of labor, the typical protocol for hourly during latent labor, every 30 minutes in active labor, every 15 in early 2nd stage and as frequently as every 5 minutes (or more often) during the few minutes just before the baby is born.
In addition to the use of a hand-held doppler or fetoscope, the labor or birth attendant uses a watch or clock to determine the fetal heart rate (FHR) in ‘beats-per-minute’ (bpm), while also noting the rhythm (regular or irregular).
In the modern era, this method of determining fetal well-being by any means (auscultation or EFM) has been expanded to include the following four parameters:
-
-
-
-
- normal baseline
- normal variability
- normal accelerations
- no pathological decelerations
-
-
-
These findings are then recorded on the mother’s chart. If at any time the rate, rhythm or other parameters are abnormal, efforts are made to determine why and necessary action is taken as indicated.
An important part of what makes hands-on monitoring work so well is the physical presence of a professionally-trained labor or birth attendant during the woman’s entire active labor and the birth. This kind of personal hands-on/eyes-on/ear-on care allows an L&D nurse or midwife to closely monitor the nature of the labor and the mother’s response to it, and then to provide specific guidance, emotional support, and encouragement and also to consult with others if questions about the unborn baby’s well-being arise.
Other Advantages of Auscultation as compared to c-EFM
There are many additional advantages of hands-on monitoring.
When laboring women are not tethered to a machine sitting next to the bed, they do not have to stay in their beds during labor. Typically women being continuously monitored are forced to lie or sit on their beds or stand in place next to their bed during the many hours of labor. But this does NOT apply to women whose baby’s are being personally monitored by the nurse or midwife using hands-on listening.
While many L&D units advertise their EFM telemetry equipment that allows women to walk around in their room and in nearby halls, most often there is only one or two of these special machines, which means they are not available to the majority of labor patients.
When the laboring woman is not hooked up to c-EFM, she becomes a free agent who can change position without being restrained by EFM belts or cautioned by the hospital staff not to move too much because it disrupts the signal.
Women being monitored by auscultation can walk around, spend time in a rocking chair, get into the shower, sit in a deep water tub, kneel over a labor ball, or squat during a pushing contraction. Being upright and mobile helps labor progress naturally and for many women makes the pain of labor tolerable without resorting to drugs or anesthesia.
By making right use of gravity throughout the first and second (or pushing) stage of labor, the use of Pitocin to speed up labor and/or operative delivery (forceps or vacuum) or Cesarean section is reduced.

Compared to auscultation, c-EFM does NOT improve neonatal outcome when used in the labors of healthy low-risk women but does result in a statistically significant increase in Cesarean surgeries.
The consensus of the scientific literature has always been clear. Beginning with the first randomized trial in 1976, and continuing with dozens and dozens of studies published since then, continuous c-EFM is only effective when used during the labors of the highest risk obstetrical patients.
 For low-risk women, the only difference in childbirth outcomes that continuous electronic monitoring makes is to increase the rate of Cesarean deliveries and all its post-operative complications including maternal mortality. Obviously, this increases the overall cost of childbirth services from a few thousand dollars to tens of thousands of dollars.
For low-risk women, the only difference in childbirth outcomes that continuous electronic monitoring makes is to increase the rate of Cesarean deliveries and all its post-operative complications including maternal mortality. Obviously, this increases the overall cost of childbirth services from a few thousand dollars to tens of thousands of dollars.
EFM ~ The Noun
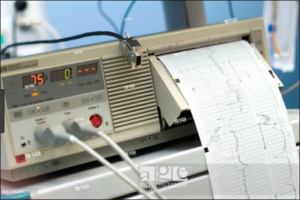 For the last four decades, American hospitals and the obstetrical profession has enthusiastically embraced the idea of hooking up a cadre of expensive electronic machines to all laboring women during every minute of the labor and birth.
For the last four decades, American hospitals and the obstetrical profession has enthusiastically embraced the idea of hooking up a cadre of expensive electronic machines to all laboring women during every minute of the labor and birth.
Unfortunately for us all, this does not square with the science and never has. One example out of hundreds of published studies is a paper written by an obstetrician for other obstetricians.
It begins with this startling statistics:
“Intrapartum fetal heart rate monitoring is the most common obstetric procedure performed in the United States.
-
- Despite the widespread use of EFM, there has been no decrease in cerebral palsy.
- … a meta-analysis of randomized control trials has shown that EFM has no effect in perinatal mortality or pediatric neurologic morbidity.2
- However, EFM is associated with an increase in the rate of operative vaginal and cesarean deliveries.1”
- Although intermittent fetal auscultation {IA} may be a theoretical option in low-risk patients, nursing staffing limitations make this impractical … ”
{Fetal Heart Rate Monitoring Update; The Female Patient, April 2011}
For the obstetrical profession to adopt c-EFM as a universal standard of care runs counter to the science as documented in high-quality research over the last four decades. For inexplicable reasons, c-EFM has become a fetish of sorts in the world of American obstetrics, one that reflects an odd and disproportionate focus on the fetus to the frequent exclusion of the wellbeing of its mother.
One example of fetus-centric thinking can be traced back to a particular obstetrical textbook: the 1974 edition of “Williams Obstetrics“. With great enthusiasm, this preface notes that the new technologies of obstetrical ultrasound and continuous electronic fetal monitoring provided the means for the obstetrical profession to achieve a long sought-after goal, which was to make the fetus the obstetricians ‘primary patient‘.
This should give pause to obstetrical patients who chose to employ and pay for an obstetrician’s service and foolishly thought they were their doctor’s ‘primary patient’.
This fetishized relationship to EFM makes it like a rabbit’s foot, religious metal, or the superpowers of the Star Wars’ robot R2D2 than a scientific medical tool. The American obstetrical system mistakenly imagines that c-EFM has the mystical power to guarantee that every newborn baby will be perfect and every obstetrician and hospital eternally protected from the expense and indignity of a malpractice suit.
 It’s hard to say whether decades of faulty logic by the obstetrical community is based on personal fears of lawsuits, a desire by hospital corporations to preserve an economic advantage or a combination of both.
It’s hard to say whether decades of faulty logic by the obstetrical community is based on personal fears of lawsuits, a desire by hospital corporations to preserve an economic advantage or a combination of both.
Irrespective of motives, the consequence has been to systemize and institutionalize the universal but nonetheless unethical use of a medical treatment that is no benefit to healthy women with normal pregnancies despite promises to the contrary.
Worse yet, the universal use of these machines introduces unnatural and unnecessary risks to the childbearing population in the United States, which is 70% to 85% of all maternity patients. The level of this unnatural risk includes an increase in preventable maternal deaths without any offsetting benefit to these mothers, their babies or to society.


