American Family Physician
 Why Are We Using Electronic Fetal Monitoring?
Why Are We Using Electronic Fetal Monitoring?
CLARISSA C. KRIPKE, M.D., Georgetown University Medical Center, Washington, D.C.
Am Fam Physician May 1999 1;59(9):2416-2422.
https://www.aafp.org/afp/1999/0501/p2416.html

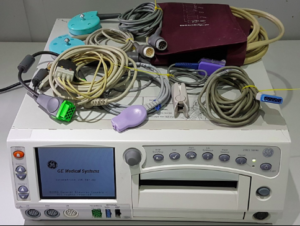
In the 1960s and 1970s, continuous electronic fetal monitoring (EFM) was introduced with the idea that it would help clinicians diagnose fetal hypoxia in time to prevent perinatal neurologic damage. By the early 1990s, more than 75 percent of the nation’s birth attendants had switched from intermittent auscultation to EFM.
1However, more recently,
a number of systematic reviews of randomized controlled trials have been published that do not support the routine use of EFM, especially in low-risk women.2–5 The data show that neurologic abnormalities are not caused by intermittent episodes of asphyxia that commonly occur during labor and delivery.The Cochrane Collaboration
2 concluded that, compared with intermittent auscultation, EFM does not reduce the rate of perinatal deaths, the rate of APGAR scores below 7 or the number of infants admitted to neonatal intensive care.
Moreover, EFM was found to result in higher rates of cesarean section (relative risk: 1.33, confidence interval: 1.08 to 1.59) and total operative deliveries (relative risk: 1.23, confidence interval: 1.15 to 1.31).
 The U.S. Preventive Services Task Force states that there is “fair” evidence that “routine EFM for low-risk women in labor is not recommended.”3
The U.S. Preventive Services Task Force states that there is “fair” evidence that “routine EFM for low-risk women in labor is not recommended.”3 For high-risk women, the task force states, “There is insufficient evidence to recommend for or against EFM . . .” The Canadian Task Force on the Periodic Health Examination made a similar recommendation.
4 A technical bulletin from the American College of Obstetricians and Gynecologists states that either EFM or intermittent auscultation is acceptable and acknowledges the risk of increased intervention with continuous monitoring.
5Furthermore, outcomes are the same regardless of whether fetal distress is managed operatively or conservatively.
6,7 Because intervention that is chosen on the basis of the fetal heart rate does not seem to improve outcomes, it is possible that we should not be monitoring by any method. Unfortunately, all of the randomized, controlled trials of EFM have compared continuous with frequent intermittent monitoring. Until we have a controlled study comparing monitored women with unmonitored women, we will continue to spend considerable health care resources without knowing whether monitoring fetal heart tones is even necessary. However, it is unlikely that this type of study will be done.
If our best evidence-based guidelines no longer recommend EFM, why are so many clinicians still using it? It seems simple to abandon a technology that has failed to live up to its promise. Nevertheless, there are educational, legal, technical and financial barriers to changing clinical practice.
First, since the advent of EFM, many nurses and physicians have not been trained in intermittent auscultation. For clinicians to feel comfortable using auscultation, more training opportunities will have to be developed.

Second, some physicians believe that EFM might still be a valuable assessment tool with better guidelines for interpreting tracings and making management decisions.
8 In this issue of
American Family Physician, Sweha and colleagues
9 review the current literature on the interpretation of fetal heart rate monitoring. However, many studies comparing the ability of experts to agree on the interpretation of an EFM tracing have shown poor inter-rater reliability, even in controlled research settings with expert clinicians.
10,11To address this problem, the National Institutes of Health and the International Federation of Gynecology and Obstetrics have established criteria for interpreting EFM strips.
12 Also, the possibility of using computer-generated interpretations to make more objective assessments is being studied.
13,14 These efforts may someday produce effective methods for interpretation and clinical decision-making. Currently, no such method exists.
Third, physicians may fear that they will be vulnerable to malpractice lawsuits if they do not use EFM. The impact of changing to intermittent monitoring on malpractice claims is unknown. However, as long as patients are counseled and intermittent auscultation is performed diligently, physicians can be confident that they are following current recommendations.
Furthermore, tracings are frequently used to justify claims that action should have been more aggressive or timely despite the fact that EFM has a low positive predictive value for fetal compromise.
15–18In one study,
19 reviewers were given two identical tracings and antenatal histories but were told that the outcome was good in one case and poor in the other. When the outcome was poor, the reviewers were more likely to disagree with the obstetrician’s interpretation and management. This study demonstrates the danger of retrospective reviews of fetal heart tracings by expert witnesses.
19,20 If hospital clinical policies support intermittent auscultation, it might prove easier to defend a management decision based on a carefully documented clinical assessment rather than on an EFM tracing.

A fourth reason that physicians may favor EFM is that many hospitals are not adequately staffed to do intermittent auscultation. Studies that show intermittent auscultation to be equivalent or better than EFM had 1:1 ratios of nurses to patients and fetal heart tones were assessed every 15 to 30 minutes during the first stage of labor and every five minutes in the second stage.
In one study,
21 a university hospital center attempted to use intermittent auscultation as the primary method of monitoring without increasing the number of staff. Auscultation was only successfully completed in 31 of 862 patients in labor with viable fetuses. Intermittent auscultation was abandoned for most patients because the staff was not able to maintain the required 1:1 nurse-patient ratio.
Reducing cesarean section rates and equipment needs might partially offset the costs of hiring additional staff to perform intermittent auscultation. Nevertheless, routine use of intermittent auscultation is likely to be more expensive than EFM. Although no data are available to indicate whether adopting intermittent auscultation reduces costly malpractice claims, it is possible that if EFM tracings were not used retroactively to question physician judgment, reducing legal costs could make intermittent auscultation financially viable. Other solutions to the staffing problems might include hiring trained birth attendants instead of registered nurses to do the monitoring. Continuous labor support has also been shown to decrease intervention and increase patient satisfaction.
22,23
Intermittent auscultation is a “high-touch, low-tech” method that lowers the number of cesarean sections performed because of fetal distress. This is safer for mothers and reduces the need for consultation, which can disrupt the doctor-patient relationship. Family physicians are at the forefront of overcoming the challenges of implementing evidence-based guidelines. They are in an ideal position to introduce intermittent monitoring to their hospitals because they often spend a significant amount of time at their patients’ bedside and usually only have one patient laboring at a time.
Dr. Kripke practices obstetrics as an instructor in the Department of Family Medicine at Georgetown University, Washington, D.C. She is a graduate of Fairfax Family Practice, a residency program of the Medical College of Virginia, Fairfax. Dr. Kripke is currently the AFP John C. Rose fellow in medical editing.
Address correspondence to Clarissa Kripke, M.D., 212 Kober-Cogan, Georgetown University Medical Center, 3800 Reservoir Rd., N.W., Washington, D.C. 20007.
REFERENCES
1. National Center for Health Statistics. Advance report of maternal and infant health data from the birth certificate, 1991. Monthly vital statistics report. 42(11) supplement. Hyattsville, MD: PublicHealth Service (no. 94-1120), 1994….
2. Thacker SB, Stroup DF. Continuous electronic fetal heart rate monitoring versus intermittent auscultation for assessment during labor. (Cochrane Review) In: The Cochrane Library, Issue No. 1. Oxford: Update Software, 1999.
3. U.S. Preventive Services Task Force. Guide to clinical preventive services, 2d ed. Baltimore: Williams & Wilkins, 1996:433–42.
4. Canadian Task Force on the Periodic Health Examination. The Canadian guide to clinical preventive health care. Ottawa: Health Canada, 1994:158–63.
5. ACOG Technical Bulletin. Fetal heart rate patterns: monitoring, interpretation, and management. No. 207. July 1995. Washington, DC.: American College of Obstetricians and Gynecologists, 1995.
6. Hofmeyr GJ. Operative versus conservative management for “fetal distress” in labour (Cochrane Review). In: The Cochrane Library, Issue 1. Oxford: Update Software, 1999
7. Pattison N, McCowan L. Cardiotocography for antepartum fetal assessment (Cochrane Review).In: The Cochrane Library, Issue 1. Oxford: Update Software, 1999.
8. Cibils L. On intrapartum fetal monitoring. Am J Obstet Gynecol. 1996;174:1382–9.
9. Sweha A, Hacker T, Nuovo J. Interpretation of the electronic fetal heart rate during labor. Am Fam Physician. 1999;59:2487–2500.
10. Todros T, Preve CU, Plazzotta C, Biolcati M, Lombardo P. Fetal heart rate tracings: observers versus computer assessment. Eur J Obstet Gynecol Reprod Biol. 1996;68:83–6.
11. Bernardes J, Costa-Pereira A, Ayres-de-Campos D, van Geijn HP, Pereira-Leite L. Evaluation of interobserver agreement of cardiotocograms. Int J Gynaecol Obstet. 1997;57:33–7.
12. Report of the FIGO Study Group on the Assessment of New Technology. Evaluation and standardization of fetal monitoring. International Federation of Gynecology and Obstetrics Int J Gynaecol Obstet. 1997;59:169–
73.
13. Electronic fetal heart rate monitoring: research guidelines for interpretation. National Institute of Child Health and Human Development Research Planning Workshop. Am J Obstet Gynecol. 1997;177:1385–90.
14. Bernardes J, Ayres-de-Campos D, Costa-Pereira A, Pereira-Leite L, Garrido A. Objective computerized fetal heart rate analysis. Int J Gynaecol Obstet. 1998;62:141–7.
15. Symonds EM, Senior OE. The anatomy of obstetric litigation. Curr Obstet Gynaecol. 1991;1:241–3.
16. Slawson D. Uncertain value of electronic fetal monitoring. J Fam Pract. 1996;42:563–4.
17. Symonds EM. Fetal monitoring: medical and legal implications for the practitioner. Curr Opin Obstet Gynecol. 1994;6:430–3.
18. Schifrin BS, Rubinstein TH. Fetal surveillance during labor: the role of the expert witness. J Perinatol. 1993;13:151–2.
19. Zain HA, Wright JW, Parrish GE, Diehl SJ. Interpreting the fetal heart rate tracing: effect of knowledge of neonatal outcome. J Repro Med. 1998;43:367–70.
20. Schifrin BS. Medicolegal ramifications of electronic fetal monitoring during labor. Clin Perinatol. 1995;22:837–54.
21. Morrison JC, Chez BF, Davis ID, Martin RW, Roberts WE, Martin JN Jr, et al. Intrapartum fetal heart rate assessment: monitoring by auscultation or electronic means. Am J Obstet Gynecol. 1993;168:63–6.
22. Zhang J, Bernasko JW, Leybovich E, Fahs M, Hatch MC. Continuous labor support from labor attendant for primiparous women: a meta-analysis. Obstet Gynecol. 1996;88(4 Pt 2):739–44.
23. Kennell J, Klaus M, McGrath S, Robertson S, Hinkley C. Continuous emotional support during labor in a US hospital. A randomized controlled trial. JAMA. 1991;265:2197–201.
Copyright © 1999 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
 Why Are We Using Electronic Fetal Monitoring?
Why Are We Using Electronic Fetal Monitoring? In the 1960s and 1970s, continuous electronic fetal monitoring (EFM) was introduced with the idea that it would help clinicians diagnose fetal hypoxia in time to prevent perinatal neurologic damage. By the early 1990s, more than 75 percent of the nation’s birth attendants had switched from intermittent auscultation to EFM.1
In the 1960s and 1970s, continuous electronic fetal monitoring (EFM) was introduced with the idea that it would help clinicians diagnose fetal hypoxia in time to prevent perinatal neurologic damage. By the early 1990s, more than 75 percent of the nation’s birth attendants had switched from intermittent auscultation to EFM.1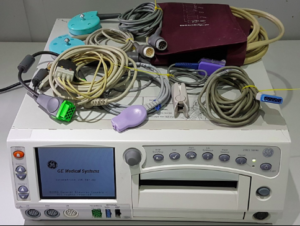 The U.S. Preventive Services Task Force states that there is “fair” evidence that “routine EFM for low-risk women in labor is not recommended.”3 For high-risk women, the task force states, “There is insufficient evidence to recommend for or against EFM . . .” The Canadian Task Force on the Periodic Health Examination made a similar recommendation.4 A technical bulletin from the American College of Obstetricians and Gynecologists states that either EFM or intermittent auscultation is acceptable and acknowledges the risk of increased intervention with continuous monitoring.5
The U.S. Preventive Services Task Force states that there is “fair” evidence that “routine EFM for low-risk women in labor is not recommended.”3 For high-risk women, the task force states, “There is insufficient evidence to recommend for or against EFM . . .” The Canadian Task Force on the Periodic Health Examination made a similar recommendation.4 A technical bulletin from the American College of Obstetricians and Gynecologists states that either EFM or intermittent auscultation is acceptable and acknowledges the risk of increased intervention with continuous monitoring.5 Second, some physicians believe that EFM might still be a valuable assessment tool with better guidelines for interpreting tracings and making management decisions.8 In this issue of American Family Physician, Sweha and colleagues9 review the current literature on the interpretation of fetal heart rate monitoring. However, many studies comparing the ability of experts to agree on the interpretation of an EFM tracing have shown poor inter-rater reliability, even in controlled research settings with expert clinicians.10,11
Second, some physicians believe that EFM might still be a valuable assessment tool with better guidelines for interpreting tracings and making management decisions.8 In this issue of American Family Physician, Sweha and colleagues9 review the current literature on the interpretation of fetal heart rate monitoring. However, many studies comparing the ability of experts to agree on the interpretation of an EFM tracing have shown poor inter-rater reliability, even in controlled research settings with expert clinicians.10,11 A fourth reason that physicians may favor EFM is that many hospitals are not adequately staffed to do intermittent auscultation. Studies that show intermittent auscultation to be equivalent or better than EFM had 1:1 ratios of nurses to patients and fetal heart tones were assessed every 15 to 30 minutes during the first stage of labor and every five minutes in the second stage.
A fourth reason that physicians may favor EFM is that many hospitals are not adequately staffed to do intermittent auscultation. Studies that show intermittent auscultation to be equivalent or better than EFM had 1:1 ratios of nurses to patients and fetal heart tones were assessed every 15 to 30 minutes during the first stage of labor and every five minutes in the second stage. Intermittent auscultation is a “high-touch, low-tech” method that lowers the number of cesarean sections performed because of fetal distress. This is safer for mothers and reduces the need for consultation, which can disrupt the doctor-patient relationship. Family physicians are at the forefront of overcoming the challenges of implementing evidence-based guidelines. They are in an ideal position to introduce intermittent monitoring to their hospitals because they often spend a significant amount of time at their patients’ bedside and usually only have one patient laboring at a time.
Intermittent auscultation is a “high-touch, low-tech” method that lowers the number of cesarean sections performed because of fetal distress. This is safer for mothers and reduces the need for consultation, which can disrupt the doctor-patient relationship. Family physicians are at the forefront of overcoming the challenges of implementing evidence-based guidelines. They are in an ideal position to introduce intermittent monitoring to their hospitals because they often spend a significant amount of time at their patients’ bedside and usually only have one patient laboring at a time.