 The start of life: a history of obstetrics by Professor J Drife, UK ~ 2023
The start of life: a history of obstetrics by Professor J Drife, UK ~ 2023
-
Correspondence to:
Professor J Drife, Department of Obstetrics and Gynaecology, Level D, Clarendon Wing, Belmont Grove, Leeds LS2 9NS, UK;
j.o.drife@leeds.ac.uk
Abstract
Obstetric intervention originally consisted of extraction of the baby, usually by the breech, to save the mother’s life in obstructed labour. Forceps, introduced in the 17th century, were later refined by men-midwives like William Smellie. In Victorian times, Simpson championed chloroform anesthesia, Lister pioneered antisepsis, and caesarean section was introduced.
In 1935, however, Britain’s maternal mortality rate was still around 400/100 000. It fell dramatically after antibiotics appeared and is now 11.4 {per 100K} In the 1960s ultrasound and electronic fetal monitoring became widely used. In 2000 the British caesarean section rate reached 20%.
Worldwide, childbirth still causes 600 000 maternal deaths a year.

Developing placenta to the left, much larger that the zygote to the right, which still has the evolutionary tail.
ORIGINS OF OBSTETRICS
The earliest birth attendants were women. In ancient mythology, goddesses (but not gods) were present at deliveries. In “primitive” tribes studied by anthropologists in the last century, the labouring woman would be accompanied by her mother or other female relative. Prehistoric figures and ancient Egyptian drawings show women giving birth in the sitting or squatting position. Birthing stools and midwives are also mentioned in the Old Testament.
 The history of obstetrics is inextricably linked with the history of midwifery.
The history of obstetrics is inextricably linked with the history of midwifery. Indeed, the first successful caesarean section in the British Isles was performed by an
Irish midwife, Mary Donally, in
1738.
1 Obstetrix was the Latin word for midwife: it is thought to derive from
obstare (to “stand before”), because the attendant stood in front of the woman to receive the baby.
Only in the 20th century did the subject taught in medical schools change its name from “midwifery” to “obstetrics”, perhaps because a Latin name seemed more academic than the Anglo-Saxon, derived from mid, “with”, and wyf, “woman”.
The writings of Hippocrates in the fifth century BC include a description of normal birth.Instrumental delivery was
restricted to stillborn babies and involved the use of hooks, destructive instruments, or compressive forceps. Such instruments were described in Sanskrit texts and were known in Arabia, Mesopotamia, and Tibet.
2 Instrumental intervention in obstructed labour probably carried a high cost in terms of maternal mortality.

Egyptian hieroglyphic of mother giving birth in the natural or “upright” position
Soranus of Ephesus (AD 98–138) described antenatal care, labour, and the management of malpresentation by internal version and breech extraction. He advised that during labour a woman should be nursed in bed until delivery was imminent, and then moved to the birthing chair, when the midwife would sit opposite her, encouraging her to push, before receiving the baby on to papyrus or cloth.
Soranus’ writings formed the basis of the “Moschion”, a Latin manuscript in the sixth century AD, but little more was added to obstetric knowledge until the invention of printing 900 years later.
THE RENAISSANCE

Traditional use of birth chair and midwife-attended birth ~ Europe, early 1600s
The first obstetric pamphlets were printed in Latin or in German in the latter part of the 15th century but made little impact. In 1513, however, an obstetric textbook appeared which became a bestseller. Der Schwangern Frauen und Hebamen Rosengarten, known as “The Rosengarten”, was translated into Dutch in 1516 and reprinted many times in Dutch and German over subsequent decades. It was also translated into several other languages, including French and English.3
“The Rosengarten” was the only published work of Eucharius Rosslin, an apothecary from Freiburg who took up medicine in 1498, worked in Worms and Frankfurt, and died in 1526. Rosslin may not have practised obstetrics himself but he restated the obstetric teaching of the ancients, including Soranus, and included new woodcuts based on their original illustrations. In his preface Rosslin berated the midwives of the time for their ignorance and superstition.

In 1532 his son published a Latin translation of the book, which became the forerunner to
De conceptu et generatione hominis, a Latin text published in 1554 by Jacob Rueff (1500–58), a surgeon and obstetrician in Zurich. Rueff’s practical experience of obstetrics improved Rosslin’s original text but the subject matter was similar to that of Soranus. Rueff described toothed forceps for extracting a dead baby (such instruments were already known in Arabia) and recommended internal and external manipulation to achieve footling presentation.
For well over 1000 years, obstetricians had managed obstructed labour by converting the presentation to a footling breech and delivering the baby by traction. Delivery of the aftercoming head, Rueff wrote, could be facilitated by pressure on the maternal abdomen. If this seems crude to us nowadays, we should remember that in the long era before caesarean section the main risk of obstructed labour was death of the mother. The obstetrician would only be summoned once the midwife realised that problems were developing, and often by that stage the baby would be dead. (The stethoscope was not invented until the 19th century, so the fetal condition could not be monitored.)
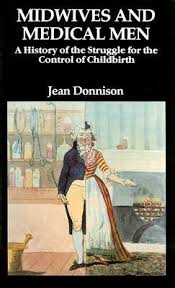
It has been suggested that the popularity of Rosslin’s and Rueff’s textbooks led to tension between doctors and midwives because doctors—barred as men from attending normal childbirth—could now learn midwifery from the printed page. If this was the reason for the emergence of the “man-midwife”, it took some time to happen. The immediate effect of the rediscovery of ancient learning seems to have been on the teaching of midwifery. During the 16th century the great French military surgeon Ambroise Paré (1510–90) founded a school for midwives in Paris.
Paré wrote about podalic version and breech extraction and about caesarean section, which he is said to have either performed or supervised not only after the death of the mother but also, at least twice, on living women. One of Pare’s pupil midwives went on to attend the French court and one of the babies she delivered—a girl named Henrietta Maria—became Queen of England at the age of 16 when she married King Charles I in 1625.
MAN-MIDWIVES

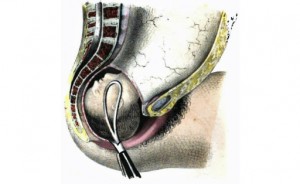
It was not until the 17th century that “accoucheurs” (male midwives) became fashionable in France. In 1663 a surgeon attended {the birth} of a mistress of Louis XIV. The best known of the French accoucheurs was Francois Mauriceau (1637–1709), whose name is familiar to today’s obstetricians by reason of the so-called “
Mauriceau-Smellie-Veit manoeuvre” for dealing with the after-coming head in a breech delivery.
This manoeuvre—almost second nature to 20th century obstetricians—involves turning the baby to face posteriorly and inserting a finger in its mouth to maintain flexion of its head. It had in fact been described several years before Mauriceau’s birth by another French accoucheur, Guillemeau. In the tradition of medical giants, Mauriceau reproduced Guillemeau’s description without any acknowledgement.
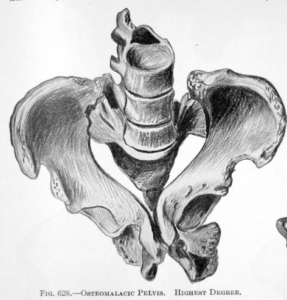
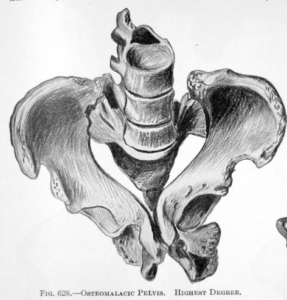
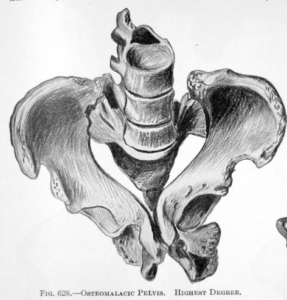
Severely contracted pelvis requiring Cesarean surgery in order to deliver the baby alive
Mauriceau had experienced obstetric tragedy on a personal level. His sister suffered antepartum haemorrhage due to placenta praevia and none of the doctors called to see her dared to attempt treatment, which of course involved internal version and breech extraction. Mauriceau himself delivered her but she died none the less.
In 1668 Mauriceau published his celebrated text, Traite des Maladies des Femmes Grosses, which was translated into several languages and went through many editions. He was indeed an innovator. He pioneered primary suturing of the perineum after delivery, “cleansing .. with red wine then applying three or four stitches”. He introduced the practice of delivering women in bed rather than on a stool. Nevertheless he remained steadfastly opposed to caesarean section, on the understandable grounds that it was almost invariably fatal to the mother.
“
Man-midwifery” reached Britain in the 17th century but remained less fashionable than in France. The most famous practitioners in this country were the Chamberlen family. William Chamberlen, a French Huguenot refugee, had fled to England in 1569 and one of his sons, Peter (1575–1628) moved to London and became surgeon to the Queen, attending the wives of both James I and Charles I in childbirth. Thus Henrietta Maria, herself delivered by a pupil of Ambroise Pare, was attended by another of medicine’s immortals. Peter Chamberlen, however, fell out with professional colleagues including William Harvey, and was arrested in 1612. It was probably Peter who developed the obstetric forceps which famously
remained the Chamberlens’ family secret for the best part of a century.
4INSTRUMENTAL DELIVERY
Peter’s eldest son, also called Peter (1601–83), became a doctor and in turn his eldest son, Hugh Chamberlen (1630–c1720) carried on the family tradition. Hugh was a close contemporary of Mauriceau and in fact translated Mauriceau’s treatise on midwifery into English. Nevertheless there was some rivalry between the two.
Hugh offered the secret of the forceps to the French government in 1670 but seems to have finally divulged it to a Dutchman, Roger Roonhuysen, in 1693, after which the forceps monopoly remained with the Roonhuysen family in Amsterdam for another 60 years. During that time, however, the secret inevitably leaked out.
The Chamberlen forceps were designed with a cephalic curve to fit around the baby’s head but lacked the pelvic curve characteristic of the modern forceps. As long as they remained a secret, the skills of Chamberlens, who carried out deliveries under a sheet or blanket, must have seemed almost magical. After the design became public knowledge, the forceps remained controversial. Initially their use was confined to some man-midwives who lived near the Chamberlens in Essex and to a few skilled specialists. Such a specialist was William Smellie, who led the way in the 18th century in establishing obstetrics as an academic discipline in Britain.
A Scotsman, Smellie (1697–1763) was born in Lanarkshire and practised there for some years before enrolling to study medicine at Glasgow University. In 1738 he went to London for training in obstetrics.
The first British school of midwifery had been founded in London in 1725 and the first Chair of midwifery in Edinburgh one year later. In 1739 Smellie went to Paris for further obstetric training but, dissatisfied with the teaching there, he returned to London and began giving midwifery courses of his own.
5 His advertisements stated that a two year course of lectures cost 20 guineas, and that “The Men and Women are taught at different hours”.
Among Smellie’s contributions were improvements to the forceps. He added the pelvic curve and adopted the “English lock”, which allowed the blades to be inserted separately into the vagina and then brought together. Again, these ideas were occurring to several practitioners around the same time. The “English lock” may have been discovered by Edmund Chapman, a man-midwife of Essex, after he lost the screw of the Chamberlen forceps in the bedclothes of one of his patients. Smellie, however, was a great teacher, and laid down rules for using the forceps which are remarkably similar to those still taught today. He published his landmark Treatise on the Theory and Practice of Midwifery in 1752.
Smellie is famous as “the master of British midwifery” but his reputation is not merely national and he has been described as one of the most important obstetricians of all times and countries. He was a man of humanity and common sense but was “sadly lacking in the social graces, and a poor conversationalist”.
He was violently opposed by some London midwives, one of whom, Elizabeth Nihell—herself trained at the Hotel Dieu in Paris and the author of a Treatise on the Art of Midwifery—memorably called him “a great horse God-mother of a he-midwife”. Smellie returned to the relative peace and quiet of Lanark in 1759. What is probably a self portrait now hangs in the Royal College of Surgeons of Edinburgh, with a copy in the Royal College of Obstetricians and Gynaecologists in London.
By the latter part of the 18th century accoucheurs were fashionable in England. William Hunter (1718–83) was another Scotsman who graduated from Glasgow University and then studied in Edinburgh before coming to London to join Smellie, who was 21 years his senior. Hunter, the older brother of the famous surgeon John, was more skilled than Smellie in the manners of polite society and at the age of 30 became Surgeon
Accoucheur to the Middlesex Hospital.
At 44 he was made consultant to Queen Charlotte and at 50 he was elected to the Royal Society. He is perhaps most famous for his Atlas of the Human Gravid Uterus.
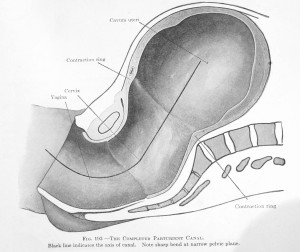
The birth canal is J shaped — long straight stem ending in the 60-degree “curve of Carus”. This arrangement is why the use of forceps is difficult. If the mother is on her back, the baby must be pulled UP (toward the ceiling) in order to come under the pubic bone and be born into the world.
Hunter exemplifies the development of obstetrics in Britain towards the end of the 18th century. Although he knew about forceps, he took pride in using them rarely and commented that his had rust on them. He praised the virtues of conservative management.
Nevertheless he was one of the first obstetricians to enter the field of normal labour, which had hitherto been the prerogative of female midwives, and this led inevitably to tension.
When Queen Charlotte was delivered in 1762 of the future King George IV, the midwife, Mrs Draper, was inside the room and Hunter was kept outside in case of emergencies. Eventually he persuaded the Queen to be rid of Mrs Draper so that he himself could conduct the delivery.
Not all Royal pregnancies had such a happy outcome. The dangers of leaving things to nature were illustrated by the tragic death in childbirth of Princess Charlotte, George IV’s only child. In 1817, at the age of 21, Charlotte went into labour with her first baby, afterwards found to be a boy weighing 9 lb. Labour began more than two weeks after the due date and lasted for 50 hours. The baby was stillborn, the placenta was removed with difficulty, and six hours later Charlotte herself died.
Forceps had been kept in readiness but were never used and indeed may not have helped. Nevertheless the obstetrician, Sir Richard Croft, was widely criticised. He shot himself a few days later and was buried near William Hunter. King George was left without an heir, and the throne passed first to his brother and then to his niece, who became Queen Victoria.
MATERNAL MORTALITY

At the start of the 19th century childbirth was still dangerous to women and it remained so, despite several advances, until well into the 20th century. Among the poor, rickets caused pelvic deformities. Maternal death affected all social classes, and across England and Wales one in 200 pregnancies ended in the death of the mother.
In maternity hospitals, however, the death rate was often much higher than this. Lying-in hospitals had been founded in cities such as London and Dublin in the middle of the 18th century, with trained midwives and accoucheurs to attend the poor. From an early stage, however, they were subject to frequent epidemics of puerperal fever, during which the maternal death rate might reach between two and eight per 100 deliveries—around 10 times the rate outside hospital.
6The contagious nature of puerperal fever had been recognised by Alexander Gordon, years ahead of his time, at the end of the 18th century. Gordon graduated from Aberdeen University in 1775 and served as a naval surgeon before studying midwifery in London and returning to Aberdeen in 1785 as probably the only accoucheur in the city. Aberdeen experienced an epidemic of puerperal fever from 1789 to 1792, and Gordon published his Treatise on the Epidemic of Puerperal Fever in Aberdeen in 1795.

He realised that
the disease was transmitted from one case to another by doctors and midwives, and that there was a
close relationship between puerperal fever and erysipelas (later found to be caused by the
streptococcus). Movingly, he wrote:
“It is a disagreeable declaration for me to mention, that I myself was the means of carrying the infection to a great number of women”.
Gordon also argued that the disease could be cured by venesection, an opinion that was accepted and widely quoted at the time, unlike his first conclusion, that the disease was contagious, which was ignored until it was rediscovered many years later.
7Eventually others reached the same conclusion, including Oliver Wendell Holmes (1809–94), the American doctor and writer. In Boston in 1843 Holmes read an eloquent paper (“ .. There is no tone deep enough for regret, and no voice loud enough for warning ..”) emphasising the doctor’s role as vector of infection, and proposing that a doctor involved in active obstetrics should never take any active part in postmortem examination of cases of puerperal fever.

Four years later, his Hungarian contemporary
Ignaz Semmelweiss (1818–65), working in Vienna, was shocked by the death of an admired professor whose finger had been cut during an autopsy on an infected case. Semmelweiss, who was struggling to understand the fearsome death rate in his obstetric unit, concluded that cadaveric material caused infection, and he made his students wash their hands in chlorinated lime between the postmortem room and the labour ward. Within months during 1847 he reduced deaths in his unit to a level similar to that in the neighbouring midwife-led unit, where staff did not attend postmortems.
Both Holmes and Semmelweiss were initially opposed and disbelieved. Semmelweiss in particular was ridiculed and discredited and he returned to his native Budapest. His monumental book Die Aetiologie, der Begriff, und die Prophylaxis der Kindbettfiebers, was finally published in 1861 but, despite his careful observations, was rambling and discursive. Unlike Holmes, he did not live to see the day in 1879 when Louis Pasteur identified the streptococcus as the cause of puerperal fever.
Meanwhile in Britain, “midwifery” had become a compulsory subject for medical students in 1833 in Scotland and 1866 in England. James Young Simpson (1811–70) was appointed Professor of Midwifery in Edinburgh in 1840. Simpson refined the obstetric forceps, producing a design that is still in use today, and also experimented with a vacuum extractor. In 1847, the year he was appointed physician to the Queen in Scotland (at the age of 36), he experimented with chloroform.
8
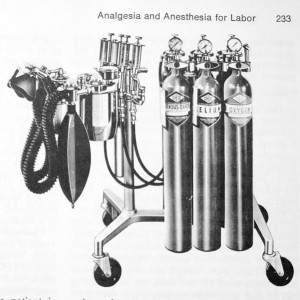
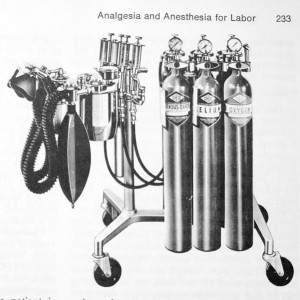
Modern equipment for providing general anesthesia
Ether anaesthesia had been discovered in January of that year. Simpson and three friends first inhaled chloroform on 4 November 1847. Four days later he administered it to a patient, a Mrs. Carstairs, who was so grateful that she named her baby girl “Anaesthesia”.
He reported the case to the Medico-Chirurgical Society of Edinburgh on 10 November 1847. Three weeks later, at the society’s meeting on 1 December, he was praising chloroform in glowing terms: “All of us, I most sincerely believe, are called upon to employ it by every principle of true humanity, as well as by every principle of true religion”.
None the less, Simpson met strong opposition from doctors and clergy, who quoted the book of Genesis: “In sorrow shalt thou bring forth children”. In 1853, however, John Snow administered chloroform to Queen Victoria during the birth of her eighth child. Chloroform became widely accepted in obstetric practice and Simpson became a baronet in 1866, choosing as the inscription on his coat of arms Victo dolore (pain conquered).
Among his many publications, Simpson recognised the contagiousness of puerperal fever almost at the same time as Semmelweiss. He did not, however, recognise the importance of the work of Joseph Lister (1827–1912), who began his experiments on antisepsis while Professor of Surgery in Glasgow in the 1860s.
9 Lister moved to Edinburgh in 1869 and may have been present when the city was brought to a halt by Simpson’s funeral in 1870.
10
Sir Joseph Lister, Surgeon to Queen Victoria; developed the principles of asepsis and surgical sterility
Listerian antisepsis, which involved the use of a carbolic acid spray, had spectacularly reduced deaths from sepsis in general surgery and was first introduced into obstetrics in 1870 in Basel, Switzerland, by Johann Bischoff, an obstetrician who had visited Lister in Glasgow. Deaths from puerperal fever in Bischoff’s hospital fell dramatically. By the 1880s Listerian antisepsis was adopted by most British and American lying-in hospitals, but at the end of that decade modern asepsis was replacing the antiseptic spray.
Towards the end of the 19th century, then, the foundations of modern obstetric and midwifery practice were being laid. Midwives were no longer illiterate “Sarah Gamps”. Several European countries introduced regulations for their training and control, though attempts to do the same in Britain failed at first. In 1872 the Obstetrical Society of London began issuing certificates of competence to midwives and in 1902 the Midwives Act made state registration compulsory and set up a Central Midwives Board to regulate the profession.
The Midwives Institute, set up in 1881, became the College of Midwives in 1941 and the Royal College in 1947.
CAESAREAN SECTION
The developments of asepsis and anaesthesia in the 19th century paved the way for the introduction of caesarean section. The name “caesarean” is probably derived, not from Julius Caesar, but from the Latin
caedere, to cut. The Roman law
Lex Caesare stated that a woman who died in late pregnancy should be delivered soon after her death, and if the baby died they should be buried separately.
The first caesarean section of modern times is attributed to a Swiss sow gelder, Jacob Nufer, who in 1500 gained permission from the authorities to operate on his wife after she had been in labour for several days. She subsequently had five successful vaginal deliveries, leading some to doubt the authenticity of the story.
After Nufer, the first caesarean sections with survival of the mother were performed in Ireland by Mary Donally in 1738; in England by Dr James Barlow in 1793; and in America by Dr John Richmond in 1827. The “first” in the British Empire outside the British Isles was performed in South Africa before 1821 by James Miranda Barry (an Edinburgh graduate who masqueraded successfully as a man from 1809 until her death in 1865), though in fact caesarean sections had been performed in Africa by indigenous healers for many years.
All these operations, however, were performed without anaesthesia. In the mid-19th century death rates remained high and caesarean section was often combined with hysterectomy. In the 1880s, with the advent of asepsis, a conservative operation was developed and the “classical” operation—a vertical incision in the upper part of the uterus—became more frequently used. This incision does not heal well, however, and in 1906 the modern “lower segment” operation was introduced, which carries less risk of subsequent rupture.
THE 20TH CENTURY
Until the 20th century obstetrics had been limited to childbirth itself, but the new century saw the introduction of antenatal care. In 1901 John Ballantyne set aside a bed for antenatal patients in Edinburgh Royal Infirmary. Antenatal clinics were opened in Boston, Sydney, and Edinburgh in 1911, 1912, and 1915 respectively. Obstetrics remained a branch of surgery until 1929, when the British College of Obstetricians and Gynaecologists was founded through the drive and ruthlessness of William Blair-Bell, who became its first president. The first college to break away from the long established colleges of physicians and surgeons, it was granted the title “Royal” in 1938 and obtained its royal charter in 1947.
The 20th century also saw developments in the technique of instrumental delivery. Although numerous obstetricians had tried to achieve fame by making minor changes to Simpson’s design, almost all forceps required the baby’s head to be facing the mother’s back and there was no effective way of dealing with deep transverse arrest. In 1916
Christian Kjelland, a Norwegian obstetrician, designed “rotational” forceps for use when the head is in other positions.
11Learning to use these forceps safely is a skill fondly remembered by today’s senior obstetricians but they are now
being superseded, as far as today’s trainees are concerned, by vacuum extractors.
12 The modern vacuum extractor (or ventouse) was invented by Tage Malmstrom of Sweden in the 1950s. It causes less maternal trauma than forceps, though it is less reliable at achieving delivery. It was initially slow to gain acceptance in Britain but eventually became popular in the 1990s.
The obstetric forceps have remained controversial throughout their history, and in the 20th century a major reason was that they were used too readily and sometimes without the necessary skill. At the end of the 19th century and during the first decades of the 20th, obstetrics formed a major part of general practice, and in the interests of efficiency a busy general practitioner would often apply the forceps rather than waiting for a normal delivery.
In response to a plea for conservatism in the British Medical Journal of 1906, several general practitioners wrote attacking elaborate aseptic precautions as unnecessary and normal delivery as impossible for “civilised” women.
One wrote: “I use chloroform and the forceps in every possible case, and have done so for many years”. This epidemic of unnecessary intervention was one of the reasons why the maternal mortality rate in Britain in 1935 was the same as it had been at the beginning of Queen Victoria’s reign.
Pregnancy has always carried a risk to the mother’s life.
 The Taj Mahal commemorates a queen who died having her 12th child in 1635.
The Taj Mahal commemorates a queen who died having her 12th child in 1635.Thomas Jefferson, the US president, lost his wife after a delivery in 1782.
Charlotte Bronte died of hyperemesis gravidarum in 1855.
In 1865 Isabella Maysom (“Mrs Beeton”) died at the age of 29 after her fourth delivery. In 19th century Britain one pregnancy in 200 led to the death of the mother and this figure still applied in the 1930s.
Britain’s maternal mortality rate, however, began to fall dramatically in 1935, with the introduction of sulfonamides. Until then, despite asepsis, nothing could be done for women who actually contracted puerperal fever. John Williams, the respected American obstetrician, commenting on suggested remedies at a meeting in 1925, said: “If you have a virulent organism and a non-resistant woman, death is the almost universal outcome, no matter what you do, and there is no use deceiving ourselves”. In the 1930s the overall death rate from puerperal fever in Queen Charlotte’s Hospital, London, was 25%.
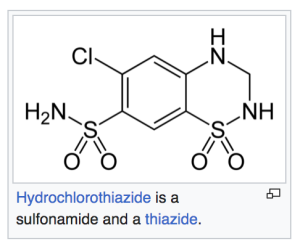
The breakthrough came with the synthesis in Germany of the
antibacterial dye sulfanilamide (Brand name
“Prontosil).
This was the result of a systematic search and the theory that a substance active against bacteria might be based on a dye because dyes adhere strongly to organic matter.
Gerhardt Domagk (1895–1964), working for the German firm Bayer, tested Prontosil, a sulphonamide, on infected mice with dramatic effect in 1932 and published his results in 1935 after the patents were secure. He was awarded the Nobel Prize for Medicine in 1939, though he did not receive it until 1947.
13Supplies of Prontosil reached London in 1936 and were tested on mice by Leonard Colebrook (1883–1967), a graduate of St Mary’s Hospital, London, who had initially worked with Alexander Fleming and had begun research on puerperal fever in the 1920s after the wife of a close friend died of the disease. Colebrook then used Prontosil, with some misgivings, on a desperately ill woman in Queen Charlotte’s Hospital. “She was watched at intervals through the night by staff `in the oddest assortment of nightwear’. The next morning her temperature had fallen from 104°F to normal”. In the first trial of 38 patients, the mortality was 8%, compared with 26.3% just before the drug was introduced.
 Sulphonamides
Sulphonamides in the form of “M&B” (manufactured by May and Baker) transformed the treatment of puerperal fever and were followed shortly by
penicillin and later by other antibiotics.
The effect on the national maternal mortality rate was spectacular and deaths from this cause almost disappeared. Later in fact, in the three years 1982–84, not a single death was recorded from infection after normal delivery, although nowadays a few cases occur each year from this cause.
Prevention maternal death from postpartum haemorrhage and criminal abortions
This success against infection was followed by efforts focused on other causes, such as the introduction of safe blood transfusion and the use of ergometrine and oxytocin for the prevention of postpartum haemorrhage.
Since 1952 the Confidential Enquiry into Maternal Deaths has examined each death in England and Wales. Its regular reports have documented a steady fall in all causes of death, beginning with hypertensive disease. By the 1960s the leading cause was sepsis after criminal abortion, which caused the deaths of around 30 women each year—most of them married and from the middle classes.
Due to the influence of Dugald Baird, safe abortion for social reasons had been available to women in parts of Scotland for some years before the 1967 Abortion Act was passed.
14 Baird (1899–1986) was professor of obstetrics and gynaecology in Aberdeen.
15After 1967, deaths from septic abortion in Britain fell, though it took 15 years before criminal abortion was abolished as a cause of maternal death.
More recently, improvements in obstetric anaesthesia, including widespread use of epidurals and the exclusion of junior trainees from the labour ward, have reduced anaesthetic deaths to almost zero. Deaths from thromboembolism have been reduced, first by ending the practice of prolonged bed rest after delivery, and more recently by improved thromboprophylaxis for women at high risk. The maternal mortality rate in Britain is now around one in 10 000, or more accurately 11.4 per 100 000 maternities.
16In developing countries, however, maternal mortality is still a major problem. In some parts of Africa beyond the reach of obstetric services the maternal mortality rate, even today, is as high as 1%. Across the globe, one woman dies of pregnancy every minute of every day. The causes are sepsis, haemorrhage, hypertensive disease, and unsafe abortion—the same causes that were common in Britain 70 years ago.
In the developed world, by contrast, in the second half of the 20th century attention shifted from the mother to the fetus. Two developments allowed this to happen. Fetal monitoring in labour became possible by detecting the fetal electrocardiogram and by sampling fetal scalp blood. These techniques were pioneered by Edward Hon, born in China but working in California, Roberto Caldeyro-Barcia of Montevideo, and Erich Saling of Berlin. Their major papers were published in the early 1960s.
The other, more important, development was obstetric ultrasound, which was developed by Ian Donald, an obstetrician, and Tom Brown, an engineer, working in the Queen Mother’s Hospital in Glasgow.
17 Donald (1910–87) graduated BA from the University of Cape Town and obtained his medical degree from the University of London, moving to the Regius Chair in Glasgow in 1954. Medical ultrasound was developed from the method used to detect submarines during the Second World War, and at first required the pregnant patient to be immersed in a bath of water. Then it was realised that water soluble jelly transmitted ultrasound waves. Donald and Brown’s first paper, with John Macvicar, was published in the
Lancet in 1958. The next 40 years saw remarkable developments of the technique, which led to the development of the specialty of fetal medicine and went on to transform other medical specialties.
Despite improvements in the safety of late pregnancy for the fetus, childbirth is still about 100 times more dangerous for the baby than for the mother. The UK perinatal mortality rate (the number of stillbirths and early neonatal deaths), having been 7% in 1935, was 0.8% in 1990.
With the safety of childbirth now generally taken for granted in Britain, the main issue for maternity care at present is the quality of the birth experience for the woman and her partner. Services are encouraged to provide choice, including home or hospital delivery, epidurals, or waterbirths. With the increased safety of obstetric anaesthesia, a few women are choosing caesarean section. The caesarean section rate is rising in many countries. In Britain it was less than 3% in the 1950s and over 20% in 2000.
18 In Rio de Janeiro it is around 90% and some people fear that this is the future for Britain. In the USA, however, it reached a peak in the 1980s at around 40% (among private patients) before falling to around 25%. Many obstetricians expect the rate in Britain to plateau around 20%–25%, with caesarean section replacing difficult vaginal delivery but not easy labour.
What of the future? Over the next decade or two, the most noticeable change in British obstetrics will be the feminisation of the specialty. Almost every one of the pioneers named in this brief historical summary has been male. At present in Britain almost 90% of consultant obstetricians are men but more than 50% of trainees are women. A small number of men have trained to become midwives. The gender difference between the medical and midwifery professions, present since the time of Hippocrates, is about to disappear.
REFERENCES
-
↵ Lawrence E. Aurelia, Cecily and Ann: a brief survey of caesarean section.
The Diplomate1996;
3:71–4.
Google Scholar
-
↵ O’Dowd MJ, Philipp EE.
The history of obstetrics and gynaecology. Carnforth: Parthenon, 1994.
-
↵ Speert H.
Obstetric and gynecologic milestones. Carnforth: Parthenon, 1996.
-
↵ Hibbard B. Pioneers in obstetrics and gynaecology 3: Peter Chamberlen.
The Diplomate1994;
1:309–11.
Google Scholar
-
↵ Studd J. Pioneers in obstetrics and gynaecology 1: William Smellie.
The Diplomate1994;
1:153–4.
Google Scholar
-
↵ Loudon I.
Death in childbirth. An international study of maternal care and maternal mortality 1800–1950. Oxford: Clarendon Press 1992.
-
↵ Loudon I.
The tragedy of childbed fever. Oxford: University Press, 2000.
-
↵ Anonymous. Obituary: Sir James Young Simpson.
Lancet1870;
i:715–8.
Google Scholar
-
↵ Anonymous. Obituary: Joseph, Baron Lister.
Lancet1912;
i:465–72.
Google Scholar
-
↵ Baskett T. Pioneers in obstetrics and gynaecology 6: James Young Simpson.
The Diplomate1997;
4:72–3.
Google Scholar
-
↵ Baskett T.
On the shoulders of giants: eponyms and names in obstetrics and gynaecology. London: RCOG Press, 1996.
-
↵ Eustace D. The origins and development of the ventouse.
The Diplomate1999;
5:260–5.
Google Scholar
-
-
-
-
↵ Lewis G, ed.
Why mothers die 1997–99. The confidential enquiries into maternal deaths. London: RCOG Press, 2001.
-
-
↵ Royal College of Obstetrics and Gynaecology Clinical Effectiveness Support Unit.
The national sentinel caesarean section audit report. London: RCOG Press, 2001.
Statistics from Altmetric.com
150 readers on Mendeley
2 readers on CiteULike
Request Permissions
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
 The start of life: a history of obstetrics by Professor J Drife, UK ~ 2023
The start of life: a history of obstetrics by Professor J Drife, UK ~ 2023
 The history of obstetrics is inextricably linked with the history of midwifery. Indeed, the first successful caesarean section in the British Isles was performed by an Irish midwife, Mary Donally, in 1738.1 Obstetrix was the Latin word for midwife: it is thought to derive from obstare (to “stand before”), because the attendant stood in front of the woman to receive the baby.
The history of obstetrics is inextricably linked with the history of midwifery. Indeed, the first successful caesarean section in the British Isles was performed by an Irish midwife, Mary Donally, in 1738.1 Obstetrix was the Latin word for midwife: it is thought to derive from obstare (to “stand before”), because the attendant stood in front of the woman to receive the baby. In 1532 his son published a Latin translation of the book, which became the forerunner to De conceptu et generatione hominis, a Latin text published in 1554 by Jacob Rueff (1500–58), a surgeon and obstetrician in Zurich. Rueff’s practical experience of obstetrics improved Rosslin’s original text but the subject matter was similar to that of Soranus. Rueff described toothed forceps for extracting a dead baby (such instruments were already known in Arabia) and recommended internal and external manipulation to achieve footling presentation.
In 1532 his son published a Latin translation of the book, which became the forerunner to De conceptu et generatione hominis, a Latin text published in 1554 by Jacob Rueff (1500–58), a surgeon and obstetrician in Zurich. Rueff’s practical experience of obstetrics improved Rosslin’s original text but the subject matter was similar to that of Soranus. Rueff described toothed forceps for extracting a dead baby (such instruments were already known in Arabia) and recommended internal and external manipulation to achieve footling presentation. It has been suggested that the popularity of Rosslin’s and Rueff’s textbooks led to tension between doctors and midwives because doctors—barred as men from attending normal childbirth—could now learn midwifery from the printed page. If this was the reason for the emergence of the “man-midwife”, it took some time to happen. The immediate effect of the rediscovery of ancient learning seems to have been on the teaching of midwifery. During the 16th century the great French military surgeon Ambroise Paré (1510–90) founded a school for midwives in Paris.
It has been suggested that the popularity of Rosslin’s and Rueff’s textbooks led to tension between doctors and midwives because doctors—barred as men from attending normal childbirth—could now learn midwifery from the printed page. If this was the reason for the emergence of the “man-midwife”, it took some time to happen. The immediate effect of the rediscovery of ancient learning seems to have been on the teaching of midwifery. During the 16th century the great French military surgeon Ambroise Paré (1510–90) founded a school for midwives in Paris. It was not until the 17th century that “accoucheurs” (male midwives) became fashionable in France. In 1663 a surgeon attended {the birth} of a mistress of Louis XIV. The best known of the French accoucheurs was Francois Mauriceau (1637–1709), whose name is familiar to today’s obstetricians by reason of the so-called “Mauriceau-Smellie-Veit manoeuvre” for dealing with the after-coming head in a breech delivery.
It was not until the 17th century that “accoucheurs” (male midwives) became fashionable in France. In 1663 a surgeon attended {the birth} of a mistress of Louis XIV. The best known of the French accoucheurs was Francois Mauriceau (1637–1709), whose name is familiar to today’s obstetricians by reason of the so-called “Mauriceau-Smellie-Veit manoeuvre” for dealing with the after-coming head in a breech delivery. Peter’s eldest son, also called Peter (1601–83), became a doctor and in turn his eldest son, Hugh Chamberlen (1630–c1720) carried on the family tradition. Hugh was a close contemporary of Mauriceau and in fact translated Mauriceau’s treatise on midwifery into English. Nevertheless there was some rivalry between the two. Hugh offered the secret of the forceps to the French government in 1670 but seems to have finally divulged it to a Dutchman, Roger Roonhuysen, in 1693, after which the forceps monopoly remained with the Roonhuysen family in Amsterdam for another 60 years. During that time, however, the secret inevitably leaked out.
Peter’s eldest son, also called Peter (1601–83), became a doctor and in turn his eldest son, Hugh Chamberlen (1630–c1720) carried on the family tradition. Hugh was a close contemporary of Mauriceau and in fact translated Mauriceau’s treatise on midwifery into English. Nevertheless there was some rivalry between the two. Hugh offered the secret of the forceps to the French government in 1670 but seems to have finally divulged it to a Dutchman, Roger Roonhuysen, in 1693, after which the forceps monopoly remained with the Roonhuysen family in Amsterdam for another 60 years. During that time, however, the secret inevitably leaked out.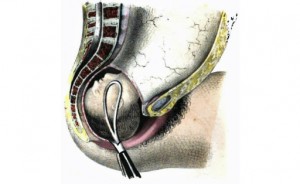 A Scotsman, Smellie (1697–1763) was born in Lanarkshire and practised there for some years before enrolling to study medicine at Glasgow University. In 1738 he went to London for training in obstetrics.
A Scotsman, Smellie (1697–1763) was born in Lanarkshire and practised there for some years before enrolling to study medicine at Glasgow University. In 1738 he went to London for training in obstetrics.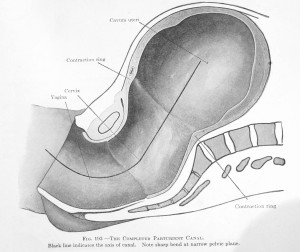
 At the start of the 19th century childbirth was still dangerous to women and it remained so, despite several advances, until well into the 20th century. Among the poor, rickets caused pelvic deformities. Maternal death affected all social classes, and across England and Wales one in 200 pregnancies ended in the death of the mother.
At the start of the 19th century childbirth was still dangerous to women and it remained so, despite several advances, until well into the 20th century. Among the poor, rickets caused pelvic deformities. Maternal death affected all social classes, and across England and Wales one in 200 pregnancies ended in the death of the mother. He realised that the disease was transmitted from one case to another by doctors and midwives, and that there was a close relationship between puerperal fever and erysipelas (later found to be caused by the streptococcus). Movingly, he wrote:
He realised that the disease was transmitted from one case to another by doctors and midwives, and that there was a close relationship between puerperal fever and erysipelas (later found to be caused by the streptococcus). Movingly, he wrote: Four years later, his Hungarian contemporary Ignaz Semmelweiss (1818–65), working in Vienna, was shocked by the death of an admired professor whose finger had been cut during an autopsy on an infected case. Semmelweiss, who was struggling to understand the fearsome death rate in his obstetric unit, concluded that cadaveric material caused infection, and he made his students wash their hands in chlorinated lime between the postmortem room and the labour ward. Within months during 1847 he reduced deaths in his unit to a level similar to that in the neighbouring midwife-led unit, where staff did not attend postmortems.
Four years later, his Hungarian contemporary Ignaz Semmelweiss (1818–65), working in Vienna, was shocked by the death of an admired professor whose finger had been cut during an autopsy on an infected case. Semmelweiss, who was struggling to understand the fearsome death rate in his obstetric unit, concluded that cadaveric material caused infection, and he made his students wash their hands in chlorinated lime between the postmortem room and the labour ward. Within months during 1847 he reduced deaths in his unit to a level similar to that in the neighbouring midwife-led unit, where staff did not attend postmortems.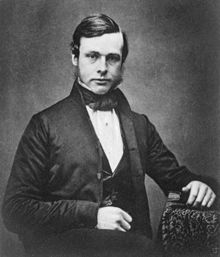
 The developments of asepsis and anaesthesia in the 19th century paved the way for the introduction of caesarean section. The name “caesarean” is probably derived, not from Julius Caesar, but from the Latin caedere, to cut. The Roman law Lex Caesare stated that a woman who died in late pregnancy should be delivered soon after her death, and if the baby died they should be buried separately.
The developments of asepsis and anaesthesia in the 19th century paved the way for the introduction of caesarean section. The name “caesarean” is probably derived, not from Julius Caesar, but from the Latin caedere, to cut. The Roman law Lex Caesare stated that a woman who died in late pregnancy should be delivered soon after her death, and if the baby died they should be buried separately.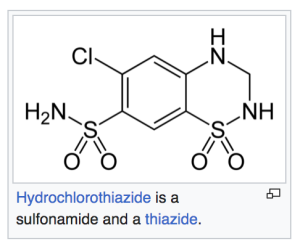 The breakthrough came with the synthesis in Germany of the antibacterial dye sulfanilamide (Brand name “Prontosil).
The breakthrough came with the synthesis in Germany of the antibacterial dye sulfanilamide (Brand name “Prontosil). Sulphonamides in the form of “M&B” (manufactured by May and Baker) transformed the treatment of puerperal fever and were followed shortly by penicillin and later by other antibiotics.
Sulphonamides in the form of “M&B” (manufactured by May and Baker) transformed the treatment of puerperal fever and were followed shortly by penicillin and later by other antibiotics.