Easy link for sharing ~https://tinyurl.com/y5gsetf6
Section 2A (of 2) ~ 1940
 How did American obstetrics stray so far from its noble foundations?
How did American obstetrics stray so far from its noble foundations?
The historic purpose of obstetrical medicine was to safeguard the life and wellbeing of laboring women under their care and relative to all circumstances of pregnancy and childbirth, both normal and complicated.
Unfortunately, the American obstetrical profession has been routinely using a technology on 100% of laboring women that is actually only safe and effective when used in the highest-risk pregnancies, which less than 15%.
Over the last four decades, dozens of scientific studies have concluded that c-EFM is ONLY effective for high-risk pregnancies. For healthy women with normal pregnancies, the routine use of EFM is both ineffective and often introduces unnecessary harm. While there is no benefit to either mother or baby, problems associated with the routine use of EFM includes increased maternal morbidity and mortality.
Continuous EFM is directly associated with unproductive cost, immobilizing of laboring women in bed, increased rate of other medical interventions, such as use of the drug Pitocin to speed up the labor and increased need for epidurals due to the increased pain associated with this labor drug.
Most detrimental of all is the dramatic increase in medically-unnecessary Cesarean sections and the many complications associated with this particular form of major surgery. These include:
- Intra-operative surgical complications such as anesthesia reactions, hemorrhage, blood transfusions and ICU admission.
- Post-op complications include infection, pulmonary embolism, a 13-fold increase in emergency hysterectomies within 14 days of the birth, re-hospitalization, and associated disruption of breastfeeding.
- Delayed complications of Cesarean surgery include drug-resistant infections, surgical adhesions, and bowel obstructions.
- Downstream complications of previous Cesarean surgery include secondary infertility and life-threatening complications in future pregnancies. This includes increased rate of late pregnancy fetal demise and maternal complications of abnormal placenta implantation that includes placenta previa and placenta accreta, increta, and percreta. This last type of abnormal placenta implantation — percreta — requires a Cesarean hysterectomy delivery and has a maternal mortality rate of 7 to 10%.
Preventing unnecessary Cesareans prevents serious complications and preventable maternal deaths.
But before addressing these extremely complex questions, it’s helpful to step back and look at the big picture from an historical perspective, and remember that our ancestors did the best they could during the many thousands of years before the discoveries of modern medical science became available to them.
A short trip in the Way-Back Machine
 This Mayday series is a search for answers. One of the questions is “How did such a great idea as obstetrics go so far off track in modern America?” In our journey to find answers, we need to fully understand the relationship that the discipline of obstetrics has with modern technologies, particularly the universal use of continuous electronic fetal monitoring (EFM) as the obstetrical standard of care in healthy low-risk labor patients.
This Mayday series is a search for answers. One of the questions is “How did such a great idea as obstetrics go so far off track in modern America?” In our journey to find answers, we need to fully understand the relationship that the discipline of obstetrics has with modern technologies, particularly the universal use of continuous electronic fetal monitoring (EFM) as the obstetrical standard of care in healthy low-risk labor patients.
To better understand the reasons behind the inappropriate use c-EFM, we need to know much more about the development of modern medical science in general, and the early history obstetrics in the US in particular.

19th century Doctor’s Black Bag – Note the two small glass bottles to the left of the doctor’s bag — one is ether and the other chloroform. Before forceps were used, the mother would be rendered unconscious with general anesthesia.
The advancing course of medical discoveries and obstetrical medicine ~ 1673 to 1950
As we think of it today, modern medical science began with the universal development of the biological sciences. The modern marriage of medical knowledge (anatomy & physiology) and the physical sciences of physics and chemistry was the discovery in 1846 of the first general anesthetic — ether — by Dr. William Morton, an American dentist from Boston.
From that point on, the scientification of Western medicine developed at an ever-quickening pace over the last half of the 19th and first half of the 20th century.
1673 ~ ‘Wee Beasties’ and other fun facts about bacteria
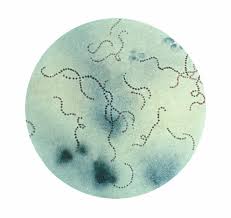 The microscopic world of bacteria were originally discovered in 1673 by a Dutch self-made scientist. Antony van Leeuwenhoek was an ordinary tradesman with little formal schooling. The only thing interesting about his earlier life was his personal friendship with the now-famous painter Vermeer (Girl with Pearl Earring) and his role as the executor of Vermeer’s estate after the artist’s untimely death.
The microscopic world of bacteria were originally discovered in 1673 by a Dutch self-made scientist. Antony van Leeuwenhoek was an ordinary tradesman with little formal schooling. The only thing interesting about his earlier life was his personal friendship with the now-famous painter Vermeer (Girl with Pearl Earring) and his role as the executor of Vermeer’s estate after the artist’s untimely death.
Fortunately for the rest of the world, van Leeuwenhoek went on to do truly extraordinary things. Using a microscope of his own invention, Antony van Leeuwenhoek was the first person to see the tiny wiggly creatures that he referred to as his “wee beasties” that we now know as microbes, which includes bacteria.
He invented the ‘scientific method’ of verifying facts thru controlled and repeatable experimentation and and is known to history as Father of Microbiology.
The Germ Theory of Infectious Disease and Contagion ~ 1881

French Chemist Louis Pasteur, inventor of ‘pasteurization, father of the Germ Theory of Infectious Diseases and contagion (1881)
It wasn’t until 1881 that the French chemist, Louis Pasteur, was able to satisfactorily prove to physician-scientists that specific strains of bacteria (ex. streptococcus, staphylococcus, etc) caused specific infectious disease and epidemics.
Prior to Pasteur’s irrefutable confirmation, medical doctors refused to believe that microscope organisms, so small as to be invisible to the human eye, were capable of causing the pathological states of infection and contagion.
Pasteur was already well known for having invented a simple process that cost nothing, did not need any specialized equipment and could be used by ordinary people to kill TB germs in raw cows’ milk by heating it to 180 degrees for several minutes. This process made it safe for children to drink fresh milk and less likely to spoil. Pasteurization obviously bore the name of its inventor.
During Pasteur’s presentation at the French Institute of Medicine in Paris in 1881, he described his Germ Theory of (Infectious) Disease, followed by an announcement that puerperal sepsis (childbed fever), which was the single largest cause of maternal death, was caused by a very specific bacteria.
Then he drew the outline of several streptococcus bacteria on a chalkboard — they looked like round railroad tanker car lined up on a train track. Pointing at this drawing, he said:
“And that gentlemen is what is killing all these women“.
The Medical Profession’s 1st Holy War between Assumptions and Evidence ~ 1840-1881
During that era, the majority of the medical profession worldwide rejected the claims by Pasteur and several others who were convinced they’d identified the role of bacteria in putrefaction and infection. The list of Pasteur’s predecessors began with Dr. Semmelweis of Vienna.
 As an assistant professor of obstetrics at the huge general hospital in Vienna — Allgemeines Krankenhaus — Dr. Semmelweis did the very first scientific study that was able to identify puerperal sepsis (childbed fever) as a contagious disease caused by some unknown, invisible substance that could be spread on the hands of doctors and medical students.
As an assistant professor of obstetrics at the huge general hospital in Vienna — Allgemeines Krankenhaus — Dr. Semmelweis did the very first scientific study that was able to identify puerperal sepsis (childbed fever) as a contagious disease caused by some unknown, invisible substance that could be spread on the hands of doctors and medical students.
Semmelweis’ carefully crafted study identified the critical chain of events in childbed fever as beginning with the daily post-mortem dissections that were core feature of medical school training. The “vector” he identified were the cadavers of new mothers and newborns, which were dissected and used as teaching cases and the hands of obstetrical professors and his medical students.
At his hospital in the 1840s, childbearing women died at an average rate of two or more each day or 700 annually. The bodies of these women and their stillborn babies were used by the obstetrical professors for instructing medical students on how to do postmortem dissections and autopsies and learn to use obstetrical procedures such as forceps deliveries.
A Brief Explanation . . .

Lying-in ward of hospital in the 1800s with dozens of maternity patients lined up on each side of the ward. Note the uniformed nurses with their ankle-length uniforms, white aprons and starched white nurse’s caps.
Before continuing, I must emphasis that these events occurred more than 180 years ago, at a time and place where no one — not even the most highly respected professors of obstetric — had certain knowledge of pathological bacteria or “germs” or understood the extraordinary concepts linking invisible bacteria and infection.
While this true account is extremely shocking, it must be seen from the perspective of its historical period, and not judged by modern standards or sensibilities.
These events occurred in a world without latex exam gloves, knowledge of microscopic pathogens, or access to antibiotics. At that time and place, the traditions associated with the clinical training of medical students were bizarre by today’s standards. These medical students were at the very bottom of the medical profession’s social ladder, and their professor expected them to do what they were told them without question.
One of those customs for doctors and med students was wiping their bloody hands on their lab coats after doing surgery or dissections. At that point in history, a doctor’s blood-stained coat was a mark of professional prestige.
Remember, this was a very long time ago and things were very different.
Austria’s largest and most famous hospital ~ Allgemeines Krankenhaus
 Clinical training at Austria’s largest and most famous hospital called for students to spend each morning in the morgue, doing autopsies and dissections on the dead bodies of obstetrical patients, the vast majority of whom had died of sepsis.
Clinical training at Austria’s largest and most famous hospital called for students to spend each morning in the morgue, doing autopsies and dissections on the dead bodies of obstetrical patients, the vast majority of whom had died of sepsis.
Then these junior doctors and their professors would dutifully wipe the blood from the last dissected body on their lab coats, rinse their hands under a cold water spigot from the pump in the courtyard, and then walk together down a short hall to a labor ward brimming with that day’s labor patients.
The students watched respectfully as their professor did a vaginal exam on each laboring woman, followed by having each medical student or intern repeat the exam. This continued until all the women on the ward had been examined 5, 6 or 7 times, while the students stood around asking questions and discussing their findings with their professor.
As was the protocols of the day, doctors and students did NOT scrub their hands with soap, running water, a good brush and antiseptic soap, nor did they rinse their hands with a germicidal solution before, between or after each patient.
The maternal mortality rate for the obstetrical department of the Allgemeines Krankenhaus wavered between a rare low of 7% and at certain times of the year, as high of 50%, with an average of two maternal deaths each day. Below is a page from Dr. Semmelweis’ records comparing maternal deaths in the two different wards of the obstetrical department, the first staffed by professors of obstetrics and their med students and the second by midwives.
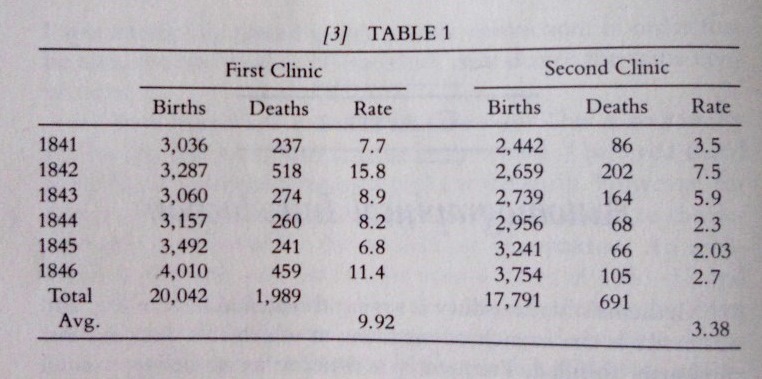
First Clinic is the medical school’s teaching ward staffed by obstetrical professors and med students who did daily autopsies and dissections; their MMR was as high as 16%. Second Clinic was the midwifery teaching ward, staffed by midwives; their students did NOT do post-mortem dissections or vag exams and had an MMR of 2% to 7.5%.
The Hand-Washing Wars: You can’t make me!
The big fight in 1840s was over the simple but critical idea of hand-washing. Despite Semmelweis’ meticulous records and irrefutable evidence, the medical staff flatly rejected his hypothesis that childbed fever was the result of invisible bacteria being carried into the labor ward on the hands of doctors and medical students. Furthermore, the idea that doctors would be forced to repeatedly wash their hands in a solution of chlorinated lime water (i.e. bleach) was insulting.
The retort by physicians of the day was to insist that “A gentleman’s hands are always clean and never cause harm to patients.”
The only wonder about this era of history is that MMR was not 100%!
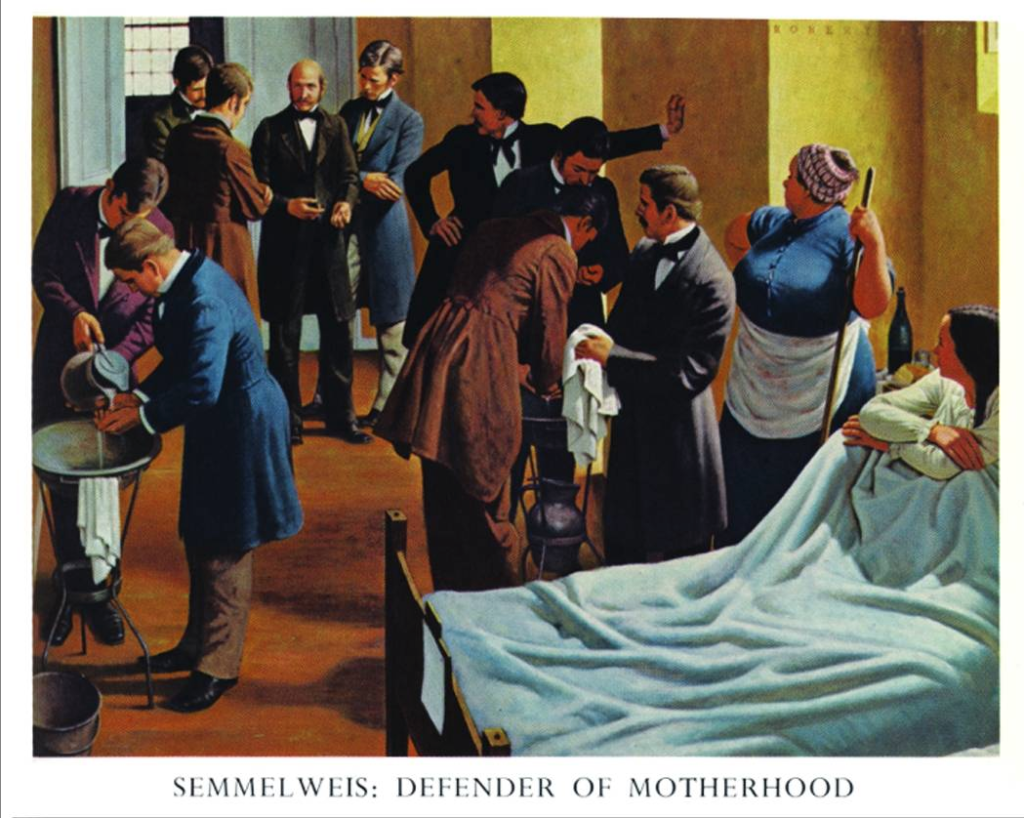
Notice the doctor disinfecting his hands as another doctor pours the germicidal solution over them and a second doctor who is wiping his hands on a clean towel.